In part one we discussed how to interpret blood tests of kidney function in the context of exercise. Today in part two we will discuss another common area of confusion and misinterpretation: the effects of exercise on liver function tests. The liver, like all of the internal organs, is quite complex and there are some considerations for evaluating blood work in those who exercise.
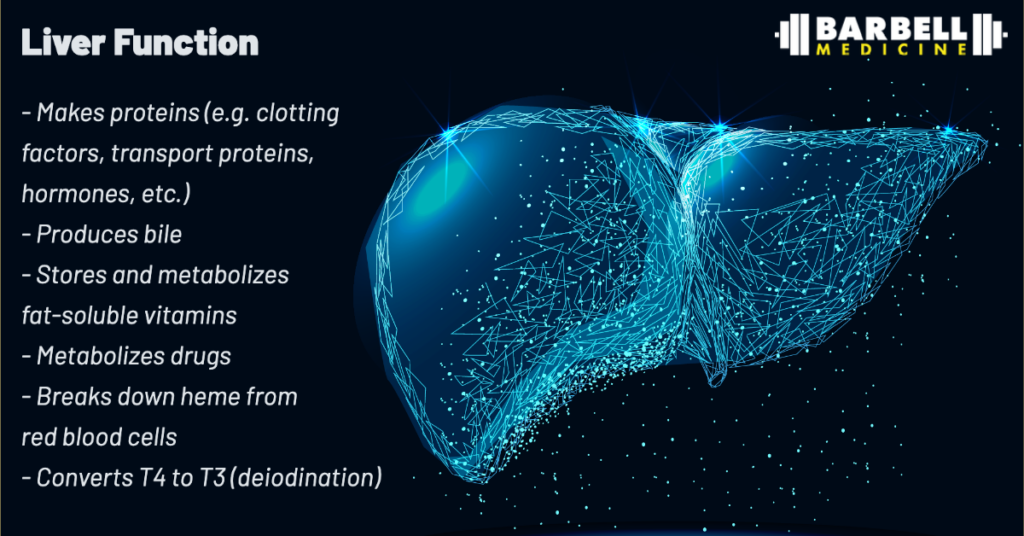
Liver Function
The liver is typically located in the right upper side of the abdomen, where it plays many important roles in the body. It produces proteins including those that help with blood clotting, transport of molecules, and certain hormones. It is involved in the breakdown and recycling of blood cells. It also participates in the digestion, metabolism, and storage of various nutrients and vitamins. The liver has a variety of enzyme systems that break down medications and toxins, including byproducts of our own metabolism as well as alcohol or other foreign substances we might consume. While people like to promote “cleanses,” typically with no supporting evidence, it is your liver that actually detoxifies your blood. These are just a few of the liver’s basic functions.
Liver-associated Blood Tests
Physicians can assess liver function in multiple ways. Let us begin with the basic Liver Function Tests, also known as a Hepatic Function Panel. This test includes blood levels of aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase, total bilirubin, total protein, and albumin. These parameters are also included alongside markers of kidney function in a Comprehensive Metabolic Panel. Abnormalities may indicate that these organs are not functioning normally, but as we established in part 1, interpretation of these values is complex, as they may be impacted by factors outside of the specific organ of interest. The body is a system and the context in which these individual components function needs to always be kept in mind.
Aspartate transaminase (AST) and alanine transaminase (ALT) are enzymes normally contained within liver cells. There is some variation and debate about what “normal” cutoff values for these tests should be, but for adults in general, normal ALT levels range from 29 to 33 units/L for males and 19 to 25 units/L for females. [1] High levels may indicate that liver cells are being injured, resulting in the release of these enzymes into the blood. Liver injury can result from fatty liver disease, alcohol use, infections, drug side effects (including certain workout supplements and anabolic steroids), inflammatory diseases, and many other causes. However, AST and ALT are also found in red blood cells, muscle, pancreas, among others. As a result, injury to these other tissues can cause AST and ALT elevations as well.
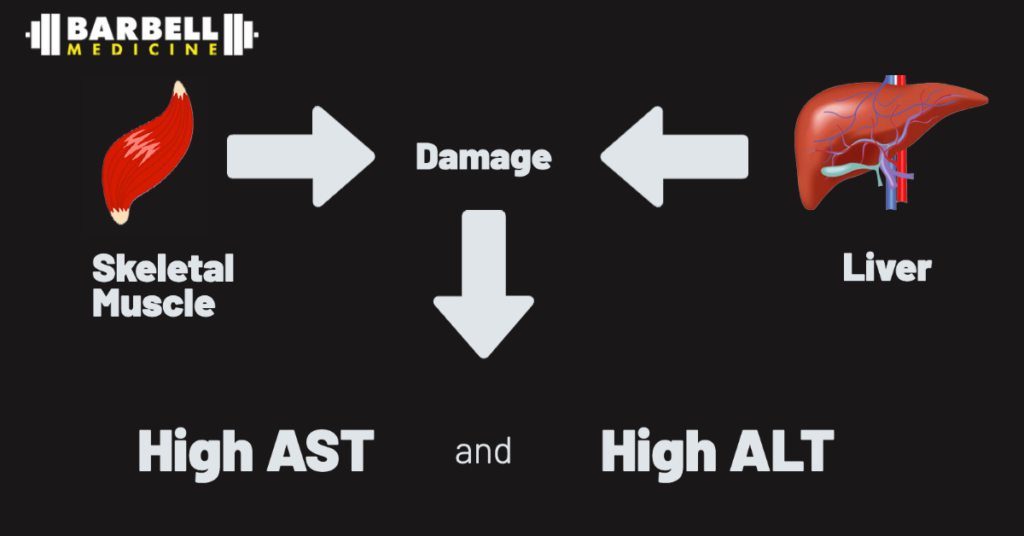
Muscle damage — whether routine, transient muscle damage caused by exercise or a condition like rhabdomyolysis, which involves rapid and extensive muscle breakdown, generally warranting a trip to the emergency room — can therefore result in high AST and ALT levels, even when the liver is healthy and functioning normally. This is a common issue for athletes undergoing blood testing in close proximity to hard training sessions or competitive efforts. One study recruited 15 healthy men without liver disease who did not habitually strength train, and had them undergo a single resistance exercise session. Their liver function markers were monitored multiple times in the subsequent days, and showed dramatic short-term elevations in AST and ALT, alongside the expected elevations in more muscle-specific tests like creatine kinase and myoglobin. Most of the elevations peaked around 3–4 days post-exercise, and gradually declined towards normal by 7–12 days, although there was significant variation between people in the study. [2]
Most clinicians interpret these elevations as solely due to liver injury, not recognizing that muscular damage from physical training may cause similar lab abnormalities. They may assume that the person has liver injury due to a harmful workout supplement, or that they are taking anabolic steroids — and in some situations this may indeed be the problem. But when they are not the cause, clinicians may initiate an extensive medical evaluation of further blood tests, imaging, and potentially invasive liver biopsies without realizing that the elevation may simply be a result of the exercise itself, and not related to the liver at all. [3]
A trained clinician should be able to assess the urgency of subsequent testing based on their comprehensive evaluation. Since other markers of liver function such as alkaline phosphatase, bilirubin, or coagulation tests that are typically not as impacted by exercise, significant abnormalities in these values require more urgent evaluation and not be dismissed as solely exercise-related. Isolated exercise-induced abnormalities can be confirmed via repeat testing after a temporary break from training. Most people’s levels will have substantially declined within 7–10 days. A smaller proportion of individuals can have persistent elevations beyond 7 days, although these should eventually normalize as well if they are related to exercise. These tests can also be paired with measurements of creatine kinase, which is a more specific marker of exercise-induced muscle damage.
Persistent elevations or further increases despite a break from training should raise concern for active inflammation or injury to the liver. This requires more thorough evaluation for conditions like fatty liver disease, gallstones, liver injury from alcohol, drugs, or supplements, viral infections, autoimmune and genetic conditions, cancer, and many other potential causes.
Interpretation of this collection of liver-associated tests is even more complex than interpreting creatinine measurements. Abnormalities may be due to emergent, life-threatening conditions, or may be benign and transient. Accurate interpretation requires knowledge of the clinical context, including who the patient is and whether they have particular signs, symptoms, or other known risk factors for disease. It is not recommended to indiscriminately check these tests in adults “just to know”; rather, they should be ordered for specific reasons, and interpreted by trained clinicians who have knowledge of the full context.
Thank you to Thomas Campitelli for his assistance in editing this article.
References
- Kwo PY, Cohen SM, Lim JK. ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries. Am J Gastroenterol. 2017 Jan;112(1):18-35. doi: 10.1038/ajg.2016.517. Epub 2016 Dec 20. PMID: 27995906.
- Pettersson J, Hindorf U, Persson P, Bengtsson T, Malmqvist U, Werkström V, Ekelund M. Muscular exercise can cause highly pathological liver function tests in healthy men. Br J Clin Pharmacol. 2008 Feb;65(2):253-9. doi: 10.1111/j.1365-2125.2007.03001.x. Epub 2007 Aug 31. PMID: 17764474; PMCID: PMC2291230.
- Tiller, Nicholas B.; Stringer, William W.. Exercise-induced increases in “liver function tests” in a healthy adult male: Is there a knowledge gap in primary care?. Journal of Family Medicine and Primary Care 12(1):p 177-180, January 2023. | DOI: 10.4103/jfmpc.jfmpc_1923_22
