Last week’s article made a strong case for embracing variability in movement for active individuals, particularly when learning a new movement. Still, much has been made of the relationship between a lifter’s back position and their risk of injury during exercise. Many coaches, doctors, and Internet experts confidently claim that lifting with a rounded lower back (i.e., lumbar flexion) during the squat or deadlift is dangerous. Sjöberg 2018 Despite this bravado, the current evidence appears less supportive than we’d expect if there was a clear relationship between these techniques and injury. In this week’s article, we’ll take a look at what the lower back is actually doing during the squat and deadlift and see if we can get to the bottom of this.
Key Points:
- Maintaining a neutral lumbar spine, the range of motion where the spine faces little resistance from tissues such as muscle, bone, and the intervertebral disc itself, during resistance training is said to be very important. Data from both animal and human cadavers suggest that exceeding as little as 35% of the lumbar spine’s flexion-extension range of motion may increase the risk of disc herniations.
- The lumbar spine moves through a substantial amount of flexion-extension range of motion in excess of 35% during compound exercises like the good morning, kettlebell, swing, and squat. Additionally, the lumbar spine also rotates and laterally flexes some amount during and between reps on the squat and deadlift.
- Disc herniation rates for resistance training tend to be lower than what is seen in sedentary populations. Additionally, it appears that regularly engaging in resistance training can reduce the risk of disc herniation compared to other activities. While resistance training likely results in disc “changes” when evaluated by advanced imaging techniques like MRI, these appear to be adaptive changes, rather than predictive of low back pain or other deleterious outcomes. That all being said, disc herniations comprise a relatively small percentage (<5%) of all primary care doctor’s visits for low back pain.
Introduction:
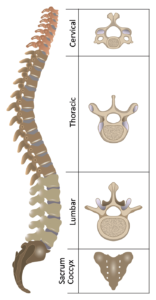
To begin, the human spine is made up of a 33 bony vertebrae that are separated into the following categories based on their location and morphology:
- Cervical (C1-C7) – The 7 most superior (e.g. higher) vertebrae make up the neck. C1 is the vertebrae closest to the skull, whereas C7 is the lowest cervical vertebra, closest to the thoracic spine. These vertebrae tend to be smaller relative to other sections of the spine and are characterized by a hole (the foramen transversarium) in the transverse processes laterally projecting off the vertebral body.
- Thoracic (T1-T12) – The 12 thoracic vertebrae connect the cervical and lumbar segments. These vertebrae are characterized by the articular surfaces seen on both the vertebral bodies and their transverse processes (except for T11 and T12) where they connect to the ribs.
- Lumbar (L1-L5) – The 5 lumbar vertebrae comprise the lower back and are the largest and thickest vertebrae of the spine. They lack the foramen transverarsium of the cervical spine and the articular surfaces for the ribs that are characteristic of the thoracic spine.
- Sacrum (S1-S5)- The 5 sacral vertebrae fuse into one segment between ages 18-30 in humans. At its lower end, it connects to the coccyx or “tailbone”, which is another much smaller fusion of 3-5 vertebrae.
Each adjacent vertebrae in the cervical, thoracic, and lumbar regions of the spine are separated from one another by an intervertebral disc (see Figure 2). Each disc has a central fluid portion, the nucleus pulposus, and an outer fibrous capsule, the annulus fibrosus. In general, the fluid portion of the disc functions takes any force applied to a vertebrae and increases the surface area that it is transferred across to adjacent vertebrae. The outer annulus fibrosus serves to contain the nucleus pulposus and overall, resist deformation of the disc. Waxenbaum 2018
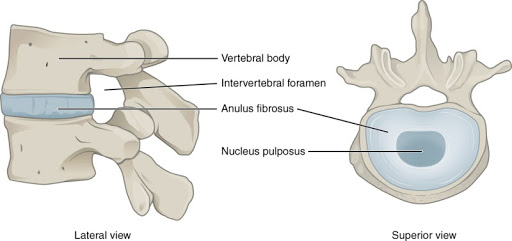
Figure 2: Anatomy of the Intervertebral Disc.
There are a total of four curvatures to the spine – one for each segment of the vertebral column. The cervical and lumbar spine are both lordotic, which refers to an inward or concave curvature of these segments. By contrast, the thoracic and sacral segments are termed kyphotic, e.g. an outward or convex curvature.
While each individual has their own anatomy, researchers have collected data to establish the following average values based on X-ray imaging:
- The average lumbar lordosis when standing at rest is ~ 41-46 degrees, with minimal difference between men and women. Vialle 2005 Hay 2015
- The average thoracic kyphosis when standing at rest is ~ 39-40 degrees.Vialle 2005
Each segment of the spine can participate in a number of different movements either in isolation or in sync with other segments. Since we’re focused on the movements made by the lower back or lumbar spine, let’s take a closer look at its specific movement capabilities.
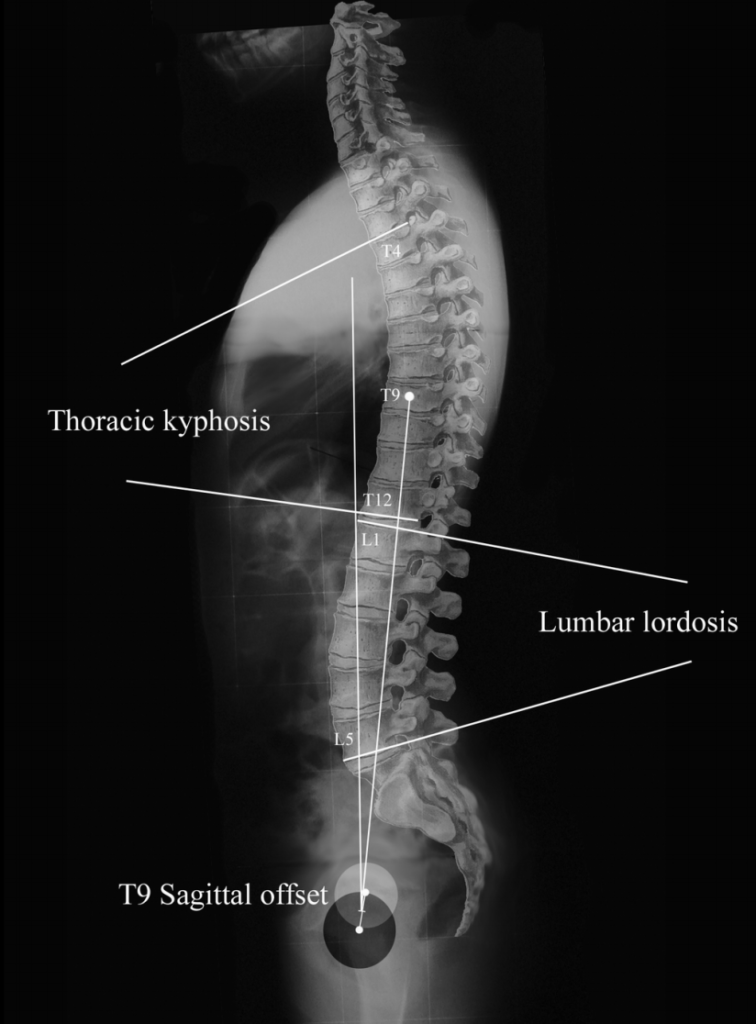
Figure 3. Lateral X-Ray of the human spine.
There are four principle actions that the lumbar spine participates in: flexion, extension, lateral flexion, and rotation. Using sophisticated electronics that were affixed to the test subjects, researchers from Yale Medical School measured average ranges of motion for each of these movements in 30 men and 30 women aged 20-70 years:
- Flexion- 54.6 degrees
- Extension- 26.6 degrees
- Lateral flexion- 17.5 degrees to the left and 19.5 degrees to the right
- Rotation- 18.2 degrees to the left and and 17.6 degrees to the right Bible 2010
These average ranges of motion are important to keep in mind as we address the concept of a neutral spine. The origin of the term neutral spine is unknown, however the earliest description in the literature comes from Panjabi, who states that the neutral zone is when movement of the spinal segments, e.g. two adjacent vertebrae, faces little resistance from tissues such as muscle, bone, and the intervertebral disc itself. By contrast, when the spine moves out of the neutral zone and faces soft tissue restraints, it enters the elastic zone. Panjabi 1992a Panjabi 1992b
The overall idea is that in this neutral zone, which changes with different postures and tasks, the load that is placed upon the spine is equally distributed across the tissues. When not in this neutral zone however, the load is unequally distributed, which may increase the risk of tissue damage to the structures comprising the spine.
Advanced imaging techniques like MRI or CT can be helpful to determine if the disc is in its normal orientation or if it should be classified as a bulging or herniated disc. For clarity, a bulging disc refers to a contained, symmetrical extension of the disc material beyond the space between adjacent vertebrae, e.g. the interspace. On the other hand, a herniated disc refers to an asymmetrical extension of the disc material past the interspace, signaling a defect in the annulus fibrosus. The herniation category also includes protrusions and extrusions, the former having a broad-based extension of disc material through the interspace and the latter having a narrowed neck compared to the rest of the disc material in the interspace.
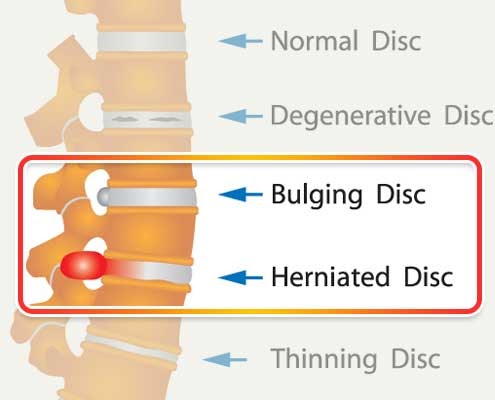
Figure 4. Bulging and herniated disc.
The prevalence of both bulging and herniated discs increase with age, as a study on over 3000 individuals without back pain reports:
- Bulging discs are found in about 30% of 20-year olds and 84% of 80-year olds.
- Disk protrusions, a type of herniation, are found in 29% of those 20-year olds and 43% of 80-year olds. Brinjikji 2014
There is substantial data supporting these common imaging findings- specifically that a disc herniation on MRI does not reliably predict current symptoms or future low back pain. Jarvik 2002 Steffens 2014 In asymptomatic individuals over 60-years for example, 36% had a herniated disc and more than 90% had a bulging disc. Allegri 2016 Additionally, only 3-4% of patients who present to their primary care physician with low back pain have a symptomatic disc herniation or spinal stenosis, e.g. a narrowing of the spinal canal. Jarvik 2002 Finally, over ⅔ of individuals with a herniated disc- symptomatic or not- will see a nearly complete resolution of the herniation after 6 months. Jordan 2009
Despite the tenuous relationship between disc herniation and low back pain, the idea that maintaining a neutral spine idea persists. There is data supporting this narrative, which are studies done in either human cadavers or dead animals where spines are dissected out of the body intact and subjected to repeated motion into and out of the elastic zone under various conditions Schollum 2018 Wade 2017 Berger-Roscher 2017 In general, these studies seem to show that flexing the lumbar spine (e.g. rounding the back) by as little as ~35% of its ROM takes it out of the neutral zone and increases the rate of disc injuries, e.g. bulging or herniation. Gooyers 2015 Callaghan 2001 Given that the average human has 55 degrees of active lumbar flexion ROM, then 19 degrees represents the 35% threshold where spines exit the neutral zone.
With that in mind, how much lumbar flexion occurs during some common exercises? On average, the lumbar spine undergoes about 26 degrees of flexion during kettlebell swings and good mornings. McGill 2012 Vigotsky 2015 Additionally, a previous study showed that there was 40 degrees of flexion that occured during a squat. Potvin 1991 All of these movements show an average range of motion outside the neutral zone, which should produce an increase in disc herniations or low back pain. However, there’s no data corroborating this relationship in live human subjects. In fact, there’s also data suggesting that discs can herniate at similar rates in the neutral zone as they do when outside of it. Veres 2010
While the lumbar spine appears to leave the neutral zone quite often during exercise, it is unclear that this increases the risk of disc herniations. It is even less clear that there is a connection with lumbar flexion out of the neutral zone, disc herniations, and low back pain. To help clear this up, we’ll take a look at how the lower back moves during deadlifts in a 2019 study, Variability of lumbar spinal alignment among power- and weightlifters during the deadlift and barbell back squat by Aasa et al.
Study Design:
This study evaluated the differences in alignment in two segments of the lumbar spine in weightlifters and powerlifters during the back squat and deadlift using motion sensors to establish this data collection technique would be reliable for spine position changes. These types of studies are commonly done prior to larger studies where researchers try to answer important clinical questions. If this data collection technique appears to be reliable, the same research group will likely do a larger trial where spine position is evaluated over a variety of different loads and rep schemes in the squat and deadlift. In this study however, individuals were asked to perform a single set of 3 repetitions at 70% of their 1-Rep Maximum (1RM).
The authors likely chose this intensity and rep scheme to reduce the chance of obtaining very noisy, unreliable data.
Subjects:
In total, 14 powerlifters (10 men, 4 women) and 10 weightlifters (4 men, 6 women) were included in the study. In order to be included in the study, each lifter had to be at least ~5 feet tall (150cm), have two years of lifting experience with the intent to compete, and not have any current injuries that limited participation. Anthropometric data can be seen in Table 1.
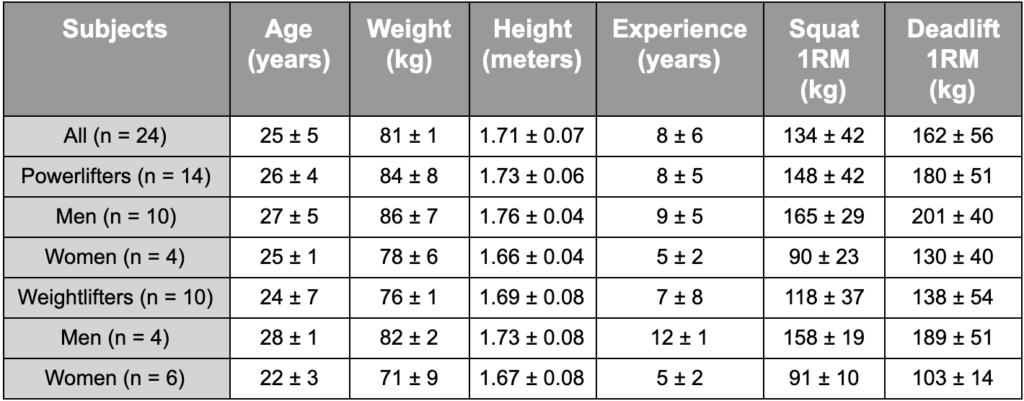
Table 1. Anthropometric characteristics of participants. Note the average experience,deadlift 1RM, and squat 1RM’s of the participants, indicating a relatively significant level of training.
Methods:
The 24 lifters were affixed with inertial measurement units (IMUs) on at the spinous processes of T11, L2, and S2. IMUs are motion sensors containing a gyroscope, accelerometer, and magnetometer that help monitoring of spinal alignment during resistance training.
For data collection, the lifters performed one set of three repetitions at 70% of his/her self-estimated 1RM for both the squat and the deadlift. All deadlifts were performed conventional, however the Olympic lifters did high bar squats and powerlifters did low bar squats. No lifting equipment other than wrist wraps were allowed.
Measurements were taken at five positions for both the squat and deadlift: (1) start position, (2) stop position (deadlift only) (3) minimum angle in degrees during each exercise, (4) maximum angle in degrees during each exercise and (5) range of motion, e.g. the difference in degrees between the min and max angles during each exercise.
Findings:
The results from this study are relatively complex, but I think if we view it as a proof-of-concept study, it’s a bit easier to understand. Remember, the primary goal of this study was to establish that the motion sensors could reliably detect changes in the spine position during the deadlift and squat. The authors hypothesized that the lifters, who were asked to perform a single set of 3 repetitions at 70% of their 1RM, would not show significant variability in the positions of their spine due to the load and repetition demands being quite light.
To assess this, the authors calculated intraclass correlation coefficients (ICC), which are a statistic to measure the reliability of a set of collected data. ICC values range from 0-1, where values below 0.5 indicate poor reliability, between 0.5 and 0.75 adequate reliability, between 0.75 and 0.9 good reliability, and any value above 0.9 indicates excellent reliability. The ICC values from the 24 subject’s deadlift and squat were all adequate or better (lowest value 0.62, highest value 1.00). This suggests that the lifters had relatively small amounts of movement variability from rep to rep. Thus, the authors successfully identified a viable strategy to measure spine position changes during the squat and deadlift.
However, it was determined that the data collection technique used made it difficult to detect lumbar position changes smaller than 4-8 degrees with respect to flexion and extension during the deadlift. For the squat, the minimum detectable difference was 4-5 degrees. In other words, a lifter had to move flex or extend their spine more than 4-5 degrees in the squat or deadlift to represent a meaningful change from rep to rep.
The average amount of flexion-extension range of motion in the lumbar spine measured during the deadlift and squat were 22 degrees and 18 degrees, respectively. While these average values suggest that most of the subjects were able to start and maintain their spines in the neutral zone, the relatively large minimal detectable difference values – 4-8 degrees in the deadlift and 4-5 degrees in the squat- suggest that some of the lifters may be starting and/or finishing their lift with a spine position outside of the neutral zone.
Additionally, spinal adjustments were made in all three dimensions in each rep for the squat and deadlift. In other words, there was some flexion-extension, lateral flexion, and rotational adjustments from rep-to-rep in most lifters.
Overall, the authors established that motion sensors can be used in this fashion to identify spine position changes that occur during the squat and deadlift. While there was relatively little spine position change from rep to rep in both the squat and deadlift, the authors were also able to determine the limitations of this data collection technique, e.g. 4-8 degrees and 4-5 degrees were the smallest spine position changes detected in the deadlift and squat, respectively.
What’s the Take Home Message?
These findings suggest that lifters are likely always making adjustments to the lumbar spine from rep to rep, even during submaximal sets. For reference, a set of 3 repetitions at 70% is about 7-8 reps shy of failure, as 70% is close to a 10RM load. Additionally, the reported lumbar spine flexion-extension range of motion, 22 and 18 degrees for the squat and deadlift, respectively, taken together with the inability to detect anything smaller than 4-5 degrees of change in both lifts suggests that many lifters may approach the end of the neutral zone, which is about 35% of the total ROM in the lumbar spine (or 19 degrees). Gooyers 2015 Callaghan 2001 This agrees with previous studies on kettlebell swings, good mornings, and squats that all showed the lumbar spine went through flexion-extension movements in excess of the 35% threshold. McGill 2012 Vigotsky 2015 Potvin 1991
Interestingly, the previous studies looked at only flexion-extension changes throughout the movements, not lateral flexion or rotation. Based on the present findings of this study, it is likely that there is substantial movement occurring both between and during each rep. The authors agree with this notion and concluded:
“In all participants during both exercises, spinal adjustments were made in both thoracolumbar and lumbopelvic areas in all three dimensions.”
Thus, it seems likely that during large, compound movements involving the lower extremities the lumbar spine is flexing and extending, rotating, and moving through lateral flexion in varying amounts. It is also likely that some, if not most, individuals will be moving past the 35% threshold that is serving as the cadaver-established cutoff for a “neutral” spine position. However, current data relating to individuals who perform these exercises do not appear to support the idea that a neutral spine position prevents disc herniations.
For example, a study looking at rates of lumbar disc herniation across specific sports by matching 287 patients with lumbar disc herniations to a control patient who was the same sex, decade of age, and who went to the same doctor’s office. The authors used a statistical analysis called “relative risk” to describe the strength of association between herniated discs and activities. A relative risk or “RR” of 1 means that the activity did not affect the outcome at all. A RR of > 1 suggests that the risk of herniation was increased by the activity, whereas a RR of <1 means that the activity decreased the risk of herniation.
When it came to using free weights at least 10 times within the past 2 years, the RR was 0.90 indicating a mild protective effect. When we look a bit closer, this same data indicates that “lifting the heaviest weights, 2 or more repetitions” had a RR value of 0.72, or significantly reduced risk of disc herniation. This was similar to most sporting activities that were studied except for bowling, which had a relative risk of 1.26. Mundt 1993
Additionally, when patients with a lumbar disc herniation are asked what they thought caused the herniation, 62% could not identify an inciting event, e.g. it was spontaneous. Of the remaining 38% who did identify an inciting event, non-lifting activities accounted for 26% of these cases while heavy lifting only accounted for 6.5%. Suri 2010
This isn’t to say that there aren’t studies indicating the resistance training doesn’t cause changes in the spine, as there are a number of different papers that report this. Vadala 2014 That being said, these changes do not reliably correlate to pain or performance metrics, as discussed in the introduction. It also bears repeating that only 3-4% of patients who present to their primary care physician with low back pain have a symptomatic disc herniation or spinal stenosis. Jarvik 2002
In summary, it does not appear that humans can avoid flexion-extension of the lumbar spine past the “neutral” zone during many exercises. Fortunately, this does not appear to increase the risk of low back pain or disc herniations, though admittedly disc herniations do not tend to correlate well with low back pain. Rather, it appears that training the back – as well as the rest of the body- through progressive overload strengthens the tissues and may reduce the risk of disc herniation in the first place.
References:
- Sjoberg, H., Aasa, U., Rosengren, M., & Berglund, L. (2018). Content validity index and reliability of a new protocol for evaluation of lifting technique in the powerlifting squat and deadlift. Journal of Strength & Conditioning Research. doi:10.1519/JSC.000000000000279
- Waxenbaum JA, Futterman B. Anatomy, Back, Intervertebral Discs. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2018 Jan.
- Vialle, R., Levassor, N., Rillardon, L., Templier, A., Skalli, W., & Guigui, P. (2005). Radiographic Analysis of the Sagittal Alignment and Balance of the Spine in Asymptomatic Subjects. The Journal of Bone & Joint Surgery, 87(2), 260–267. doi:10.2106/jbjs.d.02043
- Hay O, Dar G, Abbas J, et al. The Lumbar Lordosis in Males and Females, Revisited. PLoS One. 2015;10(8):e0133685. Published 2015 Aug 24. doi:10.1371/journal.pone.0133685
- Bible, J. E., Biswas, D., Miller, C. P., Whang, P. G., & Grauer, J. N. (2010). Normal Functional Range of Motion of the Lumbar Spine During 15 Activities of Daily Living. Journal of Spinal Disorders & Techniques, 23(2), 106–112. doi:10.1097/bsd.0b013e3181981823
- Panjabi, M. M. (1992a). The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. Journal of Spinal Disorders, 5, 383–389. doi:10.1097/00002517-199212000-00001
- Panjabi, M. M. (1992b). The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. Journal of Spinal Disorders, 5, 390–396. doi:10.1097/00002517-199212000-00002
- Schollum, M. L., Wade, K. R., Shan, Z., Robertson, P. A., Thambyah, A., & Broom, N. D. (2018). The Influence of Concordant Complex Posture and Loading Rate on Motion Segment Failure. SPINE, 1. doi:10.1097/brs.0000000000002652
- Wade, K. R., Schollum, M. L., Robertson, P. A., Thambyah, A., & Broom, N. D. (2017). A more realistic disc herniation model incorporating compression, flexion and facet-constrained shear: a mechanical and microstructural analysis. Part I: Low rate loading. European Spine Journal, 26(10), 2616–2628. doi:10.1007/s00586-017-5252-y
- Berger-Roscher, N., Casaroli, G., Rasche, V., Villa, T., Galbusera, F., & Wilke, H.-J. (2017). Influence of Complex Loading Conditions on Intervertebral Disc Failure. SPINE, 42(2), E78–E85. doi:10.1097/brs.0000000000001699
- Veres, S. P., Robertson, P. A., & Broom, N. D. (2010). ISSLS Prize Winner: How Loading Rate Influences Disc Failure Mechanics. Spine, 35(21), 1897–1908. doi:10.1097/brs.0b013e3181d9b69e
- McGill, S. M., & Marshall, L. W. (2012). Kettlebell Swing, Snatch, and Bottoms-Up Carry: Back and Hip Muscle Activation, Motion, and Low Back Loads. Journal of Strength and Conditioning Research, 26(1), 16–27. doi:10.1519/jsc.0b013e31823a4063
- Vigotsky AD, Harper EN, Ryan DR, Contreras B. Effects of load on good morning kinematics and EMG activity. PeerJ. 2015;3:e708. Published 2015 Jan 6. doi:10.7717/peerj.708
- POTVIN, J. R., McGILL, S. M., & NORMAN, R. W. (1991). Trunk Muscle and Lumbar Ligament Contributions to Dynamic Lifts with Varying Degrees of Trunk Flexion. Spine, 16(9), 1099–1107. doi:10.1097/00007632-199109000-00015
- Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811–816.
- Jarvik, J. G., & Deyo, R. A. (2002). Diagnostic Evaluation of Low Back Pain with Emphasis on Imaging. Annals of Internal Medicine, 137(7), 586. doi:10.7326/0003-4819-137-7-200210010-00010
- Steffens, D., Hancock, M. J., Maher, C. G., Williams, C., Jensen, T. S., & Latimer, J. (2013). Does magnetic resonance imaging predict future low back pain? A systematic review. European Journal of Pain, 18(6), 755–765. doi:10.1002/j.1532-2149.2013.00427.
- Allegri M, Montella S, Salici F, et al. Mechanisms of low back pain: a guide for diagnosis and therapy. F1000Res. 2016;5:F1000 Faculty Rev-1530. Published 2016 Jun 28. doi:10.12688/f1000research.8105.2
- Jordan J, Konstantinou K, O’Dowd J. Herniated lumbar disc. BMJ Clin Evid. 2009;2009:1118. Published 2009 Mar 26.
- Mundt, D. J., Kelsey, J. L., Golden, A. L., Panjabi, M. M., Pastides, H., Berg, A. T., … Hosea, T. (1993). An epidemiologic study of sports and weight lifting as possible risk factors for herniated lumbar and cervical discs. The American Journal of Sports Medicine, 21(6), 854–860. doi:10.1177/036354659302100617
- Suri P, Hunter DJ, Jouve C, et al. Inciting events associated with lumbar disc herniation. Spine J. 2010;10(5):388–395. doi:10.1016/j.spinee.2010.02.003
- Vadalà G, Russo F, Battisti S, et al. Early intervertebral disc degeneration changes in asymptomatic weightlifters assessed by t1ρ-magnetic resonance imaging. Spine (Phila Pa 1976). 2014;39(22):1881–1886. doi:10.1097/BRS.0000000000000554
