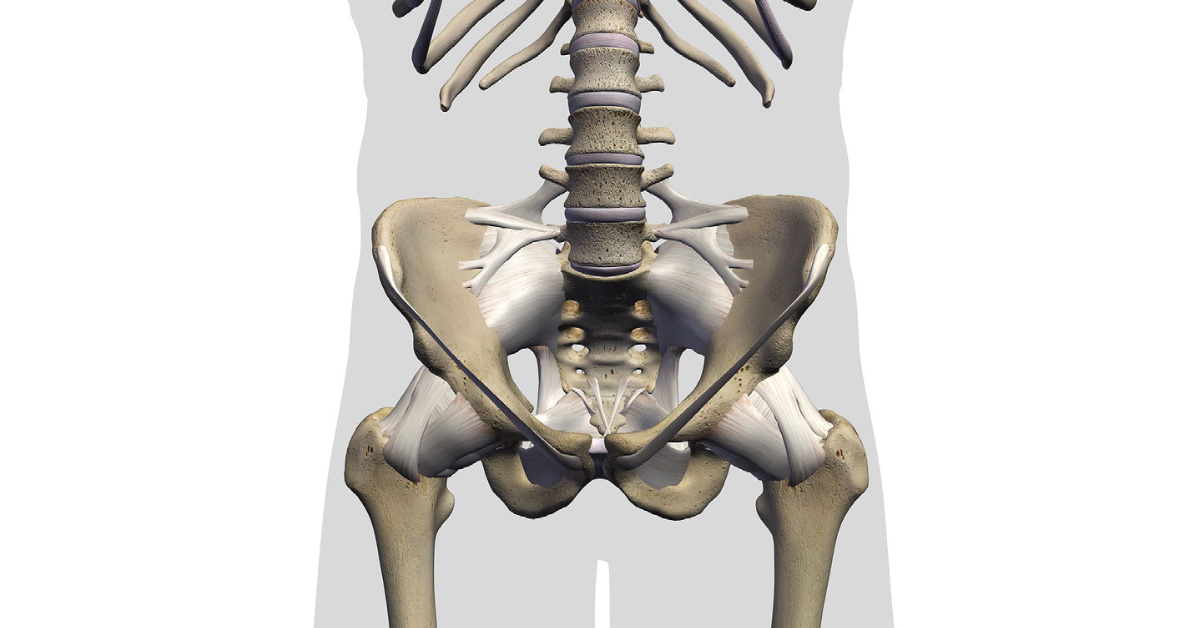
In the first article of this series we provided an introduction to the hip, discussing anatomy as well as ideas about “normal” versus “abnormal” findings of the hip. Today we will move on to discuss the first of our common diagnostic categories for hip pain: Tendinopathy. For a general overview on tendinopathy, start HERE. For a more focused discussion of tendinopathy at or around the hip, read on.
Hip symptoms that come on gradually, without a clear or sudden mechanism of injury, and are based around the origin or insertion of a muscle tend to fall in the tendinopathy category. Other diagnoses such as greater trochanteric bursitis, greater trochanteric pain syndrome or “snapping hip” syndrome can be considered here, but the overall treatment approach is the same. Management involves a combination of setting appropriate expectations, “heavy slow” resistance training, and load management. The average lifter may read the prior sentence and think “well, most of my training is already heavy and slow, so how did this happen?” Here, specific tissue does matter and sometimes training history and technical aspects can predispose someone to have symptoms in an area. At the hip, these issues often present as tendinopathy affecting the hamstrings, gluteals, hip flexors, quadriceps, and adductor muscles.
Unfortunately there are no current research papers on the implementation of heavy slow resistance training specific to hip tendinopathy. Beyer 2015, Kongsgaard 2009, Kongsgaard 2010 As a result, typical recommendations are inferred from research on the Achilles and patellar tendons. Additionally, given the numerous muscles that cross the hip joint, it can be difficult to isolate the affected tissue that needs to be worked, since other muscles can easily overcome and help complete a given task. This is by no means an advocacy for muscles having “amnesia” or “not firing”, but is merely to acknowledge that athletes are excellent at finding movement patterns that work best for them in a given moment to accomplish a task.
There do need to be some specific recommendations in terms of exercise prescription and means to attack specific areas contributing to symptoms. There is no single “normal” starting dosage for exercise; instead, each individual must find a tolerable place to start, then begin the progressive loading program from there. Since tendinopathy symptoms are related to a problem with the capacity of tissue to tolerate loading, the overall goal is to increase the area’s capacity for movement. An general example of dosing might look like the following:
Hip-Specific Exercise (specific examples will be provided below)
- Weeks 1-2: 4 sets of 12-15 at RPE 8
- Weeks 3-4: 4 sets of 10-12 at RPE 8
- Weeks 5-6: 4 sets of 8-10 at RPE 8
- Weeks 7+: 3 sets of 8 at RPE 8
These exercises should be performed at the start of the workout, as they can serve as both rehab and as the warm-up for subsequent movements. The goal here is to find an entry point into training that allows an individual to perform the desired movements. This is important because avoiding the movements with absolute rest to the area only serves to further decrease capacity for loading (detraining), and does not facilitate recovery. There still needs to be adjustment of the intensity and type of activity based on how the athlete is feeling and performing. We also commonly incorporate the use of unilateral exercises (e.g., single-leg Romanian deadlift) or controlled tempo during movements as other tools to manage overall loading (e.g., deadlift with a 3-count eccentric tempo).
It is common and expected to continue experiencing symptoms throughout rehabilitation, but there should be progressive improvement such that athletes can increasingly do more prior to feeling symptoms. For example, at week 1 an individual may be able to deadlift up to 100 kg prior to symptom onset, whereas at week 6 they are able to deadlift up to 200 kg before symptom onset. In both instances, symptoms emerge after a certain point, but there is significantly more weight on the bar — evidence of greater capacity for loading — after a few weeks of isolated training. Now, let’s get into some specifics of hip tendinopathy.
Proximal Hamstring Tendinopathy
Proximal hamstring tendinopathy is characterized by the gradual onset of pain right under the buttock. Among lifters it typically affects the deadlift and/or the squat, and in more severe instances it may affect activities like sitting and sleeping. Exercise selection is contingent upon the equipment an athlete has available. If one trains in a more “Globo-gym” setting, a prone or seated hamstring curl can be an ideal place to start in order to target the affected area in a tolerable fashion, since sticking to a competition-style deadlift will commonly result in the athlete attempting to do too much, too soon, based on expectations from their prior level of performance. The objective with using something like a hamstring curl machine is to take the affected area through a full range of motion, slowly on each leg, in order to deliver an appropriate stimulus to the affected area. For example, a 3-0-3 (3-count concentric, no isometric hold, 3-count eccentric) is a typical exercise tempo when getting started. In the event an athlete is experiencing more pronounced symptoms, they may need to start with a more limited, but tolerable, range of motion, and work towards full range of motion as symptoms improve. Individuals with a tendency to load too aggressively may also need to restrict the tempo even further, for example 6-0-6 or 5-1-5, or increase the target rep range.
An athlete who trains primarily in a powerlifting style gym may need to use a Romanian deadlift or stiff legged deadlift, with the goal of feeling tension in the affected area. Unilateral movements such as single-leg suitcase deadlift or single-leg Romanian deadlifts may play a role here as well, particularly for those who tend to “overshoot” and use excessively heavy loads. Attempting to rehab a single-leg using a double leg movement can make it more difficult to isolate the affected area to ensure it is receiving the desired stimulus. If a single leg deadlift is chosen, holding on to a rack can aid in balance to help focus on maintaining tension throughout each repetition.
Gluteal Tendinopathy
Gluteal tendinopathy is typically characterized by pain over the lateral hip. While most athletes tend to think of their glutes more as their traditional buttocks, what would qualify as a tendinopathy is where the muscles insert into the greater trochanter on the outside of the hip. An athlete who trains in a “Globo-gym” setting may benefit from starting with the hip abduction machine. This can be done seated or in standing with the goal of a slow, full range of motion contraction. For an athlete who trains in a powerlifting-style gym, there are other options. The main three to implement are a curtsy lunge, a lateral step-down, and a pistol squat to a lower depth. The main goal is to find a means to target the lateral hip in a tolerable fashion using the available equipment on hand. It should be stressed that there is no single exercise that works well for everyone as they progress through symptoms, and some trial and error may be needed to find each individual’s tolerable entry point.
Both gluteal and hamstring tendinopathy can be difficult from a treatment perspective because there are multiple muscles attached at the site of symptoms. Specific loading may therefore involve experimenting with range of motion or technique in order to isolate the affected area. While part of the approach is to drive tissue specific adaptation, the other part is also graded exposure to allow the tissue to become less sensitive. Attempting to rehab exclusively with large, bilateral, compound-type movements gives powerlifters an opportunity to compensate for the affected tissue and inappropriately overload the area, increasing the risk of symptom flares and ongoing pain issues.
Quadriceps Tendinopathy
Although quadriceps tendinopathy is characterized by symptoms located just above the kneecap rather than at the hip, it is worth including in our outline of recommendations. Limiting anterior tibial translation (how far the knee moves forward) can be helpful in the early stage of rehab, when things are particularly sensitive. In the Globo-gym setting a leg press is an excellent place to begin, being mindful of knee translation by starting out with the feet towards the top of the machine. In both the powerlifting and Globo-gym settings, lunges or split squats can be another starting point. Athletes can start with their shin up against a bench to limit how far forward their knee can move. As symptoms begin to improve, they can move their foot back to allow for more forward knee movement as the area becomes less sensitive.
The goal in this instance is NOT to limit or constrain a motion indefinitely, but rather to work within a tolerable range and reintroduce more range of motion as symptoms subside. Within the range of tolerable symptoms however, the weight used should be relatively challenging and the tempo should again be slow and controlled. The emphasis should be on placing the affected area under tension, not on the absolute weight lifted (remember: no one cares how much weight you split squat during rehab).
Hip flexor Tendinopathy
Hip flexor tendinopathy is characterized by the gradual onset of pain in the front of the hip, particularly when the muscles in that region are placed under tension. Our recommended initial exercise in this situation is a Reverse Nordic curl. The recommended rep scheme changes for this exercise compared to the general template outlined above, since it is typically performed with just bodyweight. The goal is to be able to go further back as symptoms improve and the athlete gets stronger in the movement. Typical schemes are 4 sets of 6 repetitions through a tolerable range of motion. Athletes can also use a rear-foot elevated split squat, where the leg experiencing symptoms is elevated and the goal is to get tension on the hip flexor region of the back leg as the athlete descends into the squat.
Each of these are suggestions for entry points and these are not universal guarantees of effectiveness. What may work for some athletes to start may not work for others, but this set of suggestions is a good place to begin program alterations.
Adductor Tendinopathy
Adductor tendinopathy is characterized by the gradual onset of pain in the groin. This can affect the bottom position of the squat, as well as the conventional or sumo deadlifts. While there are no papers directly related to adductor tendinopathy, we do have research on loading programs for more general adductor-related groin pain. Yousefzadeh 2018 In one study, athletes with longstanding groin pain underwent a tiered protocol of progressive loading to strengthen the adductors and abductors based off a protocol originally designed over 20 years ago. Holmich 1999 Progressive loading to treat symptoms is by no means a new concept, it is more often poorly implemented due to inadequate exercise dosing and intensity for the individual. Athletes began with a series of isometric adductor work and trunk exercises to train specific muscle groups. As symptoms improved, they progressed to a program of 5 sets of 10 strengthening exercises, with the load chosen by the clinician. Of the athletes in the cohort, 78% were able to return to their respective sport just over 14 weeks. This is more evidence that simple loading protocols can elicit positive results. The same cohort also demonstrated a greater than 20% improvement in isometric adductor and abductor strength and a greater than 7% increase in eccentric strength.
Athletes experiencing symptoms in this region would benefit from a loading protocol based on a lateral lunge. In the same fashion as with other tendinopathies, the goal is to load within a tolerable range of motion and slowly increase both weight and the range of motion through which the athlete can move. In a Globo-gym environment an athlete could also opt for using an adductor machine. The emphasis being on some isolated work on the sensitized area.
In this article we’ve reviewed the typical presentation of tendinopathies around the hip, including hamstring, hip flexor, quadriceps, and adductor tendinopathies, as well as provided practical recommendations for how to approach the rehab process. This article is not a comprehensive treatment of the topic, and if an individual is unable to achieve relief with the above recommendations, they can reach out to the Pain and Rehabilitation team for consultation and further assistance.
So far we’ve covered the approach to managing tendinopathies around the hip, which commonly affect the hamstrings, adductors, hip flexors, and quadriceps. In the next article of our series we’ll move on to discuss the approach to acute muscle injuries (commonly known as “muscle strains”) around the hip.