Performance in specific sports requires specific adaptations, while developing overall physical literacy and athletic power is predicated on a broad range of traits. If an individual is meeting the base physical activity guidelines as either a youth or an adult, the minutiae of small asymmetries does not warrant further attention. Some sports have shown asymmetries to be common in baseball players, demonstrating differences in range of motion of both their shoulders and hip.Oliver 2016 It would not make sense for a sweep rower to demonstrate the same degree of rotation side to side if they have rowed starboard for their entire career. However, after an injury, there are instances where asymmetries have been shown to play a role in the risk of reinjury.Fousekis 2011, Rambaud 2018 The current piece will serve as a scoping review for those instances, as well as discuss the evidence on how well we are addressing the issue in these situations.
Key Points:
- Strength testing using manual muscle tests is grossly insufficient for determining return to sport readiness as it lacks precision and sensitivity.
- Dynamometry can be an effective tool for determining strength deficits side to side and tracking progress through return to sport.
- If an athlete does possess an asymmetry after injury, that likely means they need to be doing more work in their programming to address this in a constrained manner.
Defining terms will be important as some of the vernacular may be unfamiliar to the lay reader. Below will be common terms used throughout this piece and their associated acronyms.
- Limb Symmetry Index (LSI): The percentage difference in strength side to side for a specific muscle group or limb. The calculation is performed by dividing the affected side by the unaffected side. For example, an athlete kicking 85 pounds on their surgical leg and 120 pounds on their nonsurgical leg would have a quadriceps index of 70.8%.
- Peak Torque to Body weight ratio (PT/BW): The ratio of the peak torque (in Newton-meters) to body weight (in kilograms). This can be an important conversion if an athlete has been away from activity for a while, as a decrease in unaffected leg strength can make limb symmetry indexes appear better than reality.
- Hamstring to Quad ratio (H:Q ratio): An antiquated, unsubstantiated metric that was used in the early 2000’s to push narratives such as “quad dominant” athletes.
- Manual Muscle Test (MMT): A test used to assess the strength of a muscle on a 0-5 scale. The test is performed with an athlete resisting a clinician’s force. There is a high degree of subjectivity in the grades greater than 3/5, and rating is contingent upon both the strength of the clinician and that of the athlete.
- Precision: the degree to which repeated measurements demonstrate the same result. The classic example used to delineate precision versus accuracy is a dart board. If the goal is to hit a bullseye, someone hitting triple ten three times would be very precise, but would not be accurate. The issue with precision in terms of manual muscle tests is once an individual can resist “strong pressure” it is impossible to be precise beyond “did they hit the dartboard” to the analogy above.
- Accuracy: the degree of closeness of a measurement to the true measurement. If the goal is to hit a bullseye, accuracy would be the proximity of each throw to the bullseye.
Before we address the instances in which symmetry matters, I want to make clear that for the general population it is far more important that physical activity guidelines are met than searching out asymmetries on an initial assessment. There are conflicting data on the percentage of the population currently meeting these guidelines, but overall the research supports that getting people to move confers far greater benefit than whether their quadriceps index is greater than 90%.
The issue that often arises when discussing strength is how it is defined and measured. We will adopt the definition proposed by Bohanon of “the maximum voluntary resultant output that muscles can bring to bear on the environment under a specific set of test conditions.” Bohannon 1987 Often, an arbitrary metric such as a single-leg squat or manual muscle test is used to assess quadriceps strength, but this is grossly insufficient for precision.
Muscles such as the quadriceps should be able to generate a large magnitude of force, and a clinician merely pushing against a leg will often not be able to generate enough force to detect weakness. Even if they can detect weakness, they will not be able to ascertain the specific degree of weakness. Similarly, the issue with a single-leg squat is that it allows other muscles to assist in the performance of the activity, and requires a degree of skill as well. An athlete may not be able to perform the task due to the novelty, or they may perform very well due to frequently practicing the task, increasing the risk of a false negative test for specific strength deficits. Bohannon proposes that any measure of strength should fulfill 4 criteria:
- They must be sensitive enough to distinguish sub-normal from normal strength
- They should be precise enough to document both increases and decreases in strength
- They should be reliable
- They should be predictive of other variables of potentially greater importance
We will defer the conversation of what constitutes “normal” strength for now, as this would constitute a piece unto itself since there is a wide range of “normal” contingent upon the goals and background of each athlete. For the second point, the precision should be quantifiable and not based on a clinician’s subjective determination. For example, if an athlete is initially able to perform one body weight squat and can now perform two, did they become stronger or more skilled? There is also a component of validity in the discussion of a particular muscle being tested. There is no feasible way to isolate a gluteus medius or a vastus medialis with a test, and therefore declaring them as weak unto themselves needs to stop as a narrative as it is not valid. What is lost in precision and validity of a particular muscle can be gained in accuracy of movement by discussing strength in terms of range of motion i.e. hip abduction or knee extension.
The Problems With Manual Muscle Testing
In the often-used manual muscle test format, it is likely many athletes would test as “normal” strength in their quadriceps. The format used in most orthopedic/sports settings is a scale ranging from “zero” where no palpable contraction can be felt to “five” which is holding against “strong” pressure. The scale does not offer good means with which to discern side to side strength differences or gradations in strength changes.
From Table 1, if an athlete can move through range of motion against gravity, they test as a 3 out of 5 for strength. Beyond that, vernacular such as “slight pressure,” “moderate pressure” and “strong pressure” are introduced into the grading scale. This creates multiple problems as there is 1) no precision in what constitutes slight, moderate, or strong within or between clinicians 2) it is likely predicated upon the strength of the clinician performing the test as if the goal is to “break,” it presupposes that the clinician is stronger than the athlete. In this light, telling an athlete who squats 2.5 times their bodyweight to full depth that their glutes are “weak” is asinine.
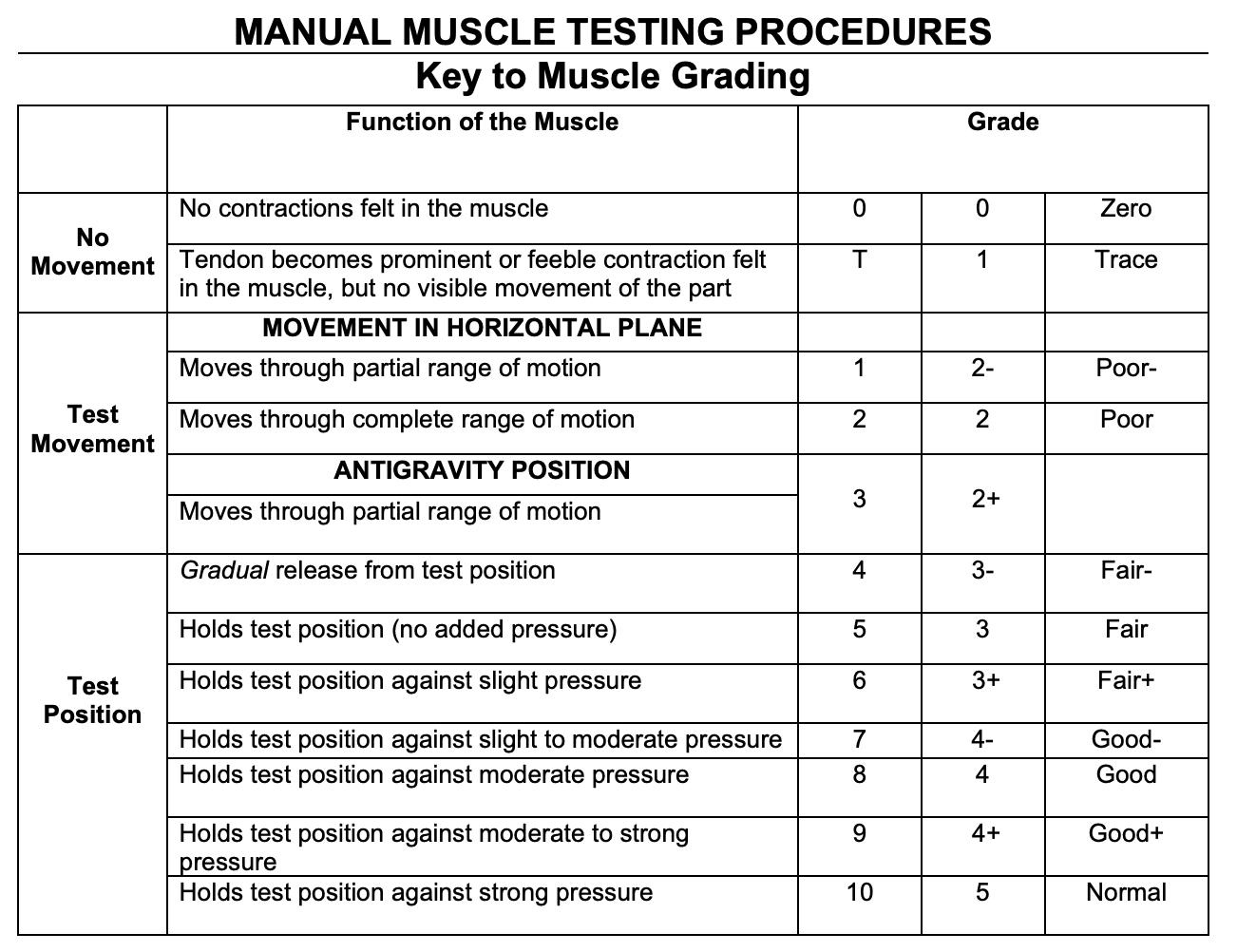
Once an athlete can resist against “strong” pressure, there is nowhere else to go. But, if that athlete’s sport is predicated on producing maximum force such as sprinting, jumping, or powerlifting, when is “strong” pressure strong enough? Framed another way, at what point would a deficit in strength either decrease an athlete’s performance, or increase their risk of injury? The answer to that question is much more ambiguous given a lack of good evidence to guide us.
If strength is to be used as an outcome measure, it needs to be accurately assessed with the gold standard method of dynamometry.Osternig 1986 The devices range from the cumbersome Biodex machines, often used for isokinetic testing in research facilities, to handheld and pull dynamometers more applicable to a typical clinic or gym setting.
Isokinetic dynamometers resist force, controlling speed at a predetermined rate. Typical measurements in the literature for the knee are taken from 60 degrees/second, 180 deg/s, and 300 deg/s but this can be varied according to joint and speed. This means that if an athlete is on an isokinetic dynamometer, no matter how hard they push against the device, it will only move at the aforementioned speed.
Handheld dynamometry is typically used to measure isometric force. Both devices allow for strength to be tested on a granular level. Still, with handheld dynamometry, the strength of the therapist applying the force may still influence the outcome if they have not secured the device to another object.
Isometric testing allows for maximal force production, but no matter the force into the dynamometer, it remains stationary.
When it comes to assessing strength, medical and rehabilitation professionals generally do a poor job of determining when an athlete possesses sufficient capacity to return to sport. A classic example of requiring a certain level of strength prior to returning to sport is after ACL reconstruction (more on this specific instance later). Two studies by Greenburg et al surveyed rehab professionals and surgeons for their return to sport clearance criteria after ACL reconstruction. Greenburg 2018, Greenburg 2019 The first study looked at physical therapists who were members of the orthopedic or sports societies and their metrics for clearance of return to sport. Of those, 80% reported using “strength” as a metric for determining readiness for return to sport.
Yet, 56% of that cohort only used manual muscle testing as a determinant for readiness. Clinicians and fitness professionals often want to get in the weeds on muscle imbalances, but even in the few instances where we have an established need to address them, few are actually checking with any degree of rigor. Physicians fared no better. In the second study, members from the pediatric research in sports medicine (PRiSM) society were asked the same question. Here, 100% of respondents reported using “strength” as a metric for clinical decision making, however 60% used MMT, 28% isokinetic testing, and 12% isometric testing. To reiterate, of those clinicians taking the time to test muscle strength prior to clearance for return to sport, over half were using a method not shown to be reliable in discerning weakness between sides.
In practical terms, a standard assessment of MMT for knee extension would involve an athlete sitting on the edge of the bed and kicking out into a clinician’s hand sitting in front of them. If an athlete was able to kick out 150 pounds on one leg, and 120 pounds on the other, they would have an 80% LSI — but this depends on the clinician being able to discern that 30 pound difference. This is highly unlikely and would be even more problematic if an athlete were kicking out 200# with one leg and 140# with the other. Now, they would have a 70% LSI, but it is unlikely that many clinicians would be capable of picking this up as 140# would likely exceed the force they could generate against the athlete with their hands.
When Strength Matters
Strength metrics come into play when entering the discussion of reinjury rates. Currently, instances for which limb symmetry index influence return to competition that we will discuss include after a muscle injury and after surgery. Recent reinjury rates for muscle injuries varies between 10.1% for hip flexor and quadriceps injuries and 34% for hamstrings. Eckard 2017, Schmidtt 2012 For athletes after ACL reconstruction, the reinjury rate is 23%.Wiggins 2016 With a rate of subsequent injury that high, research on means to reduce that rate continue to evolve.
The movement away from absolute rest has created a spectrum of return to sport activities. The first phase involves foundational rehabilitation, utilizing a structured program within the constraints of the injury to address identified deficits. Within this, an athlete is often able to return to participation in activities related to their sport. For a powerlifter, this would mean returning to the primary movements of squat, bench press, and deadlift. Contingent upon the injury, there is a high likelihood that at least one of the lifts can be trained normally through a rehabilitation process. For example, an athlete post-knee surgery may be limited in their squatting, but there is often no reason they cannot continue to bench press. Post-shoulder surgery, an athlete will likely be able to squat with a safety bar prior to getting into a high or low bar position, but they are still participating in the sport.
Once the constraints of the initial injury are removed, then an athlete can return to practice. For a lifter, this would mean returning to the three primary lifts, but with new constraints on training intensity and volume. After a muscle or tendon repair, the movements should be reintroduced prior to heavy loading. This may involve capping RPE or absolute weight on the bar. A squat with an empty barbell is still more of a step towards recovery than not squatting at all. It is only after going through these progressions that return to sport should occur, but metrics need to be in place in terms of both healing parameters of tissue and return of capacity for strength prior to moving between categories.
Many assessments used for return to sport criteria are exposed to Goodhart’s Law, which states “when a measure becomes a target, it ceases to become a good measure.” The single-leg squat example would fit this as a clinician or coach, knowing it is an outcome measure, could work to develop the skill in an athlete. The same principle can hold true for other metrics typically included in return to sport testing, as hop tests have shown a weak association with “normal” landing biomechanics after ACL reconstruction.Wren 2018 The discussion of what constitutes “normal” and what deviation from that norm is acceptable again emerges but is beyond the scope of this piece. As should be evident by now, return to sport decisions are complicated and the metrics used are often insufficient to inform clinical decisions with a high level of confidence.
For both muscle injuries and after ACL reconstruction, higher limb symmetry indexes have demonstrated protection against re-injury. A study from Sanfilippo et al attempted to discern hamstring morphological and strength differences after an injury utilizing MRI and isokinetic testing.Sanfilippo 2014 For this cohort, at return to sport (RTS) there was 20.4% decrease in cross sectional area in the hamstring of the injured limb compared to the uninjured limb. Strength testing revealed a 9.6% difference in peak torque for the affected limb that had diminished by 6-months. This demonstrates that strength is not a 1:1 ratio with cross sectional area, but more importantly that a deficit persists at RTS.
Two papers by Fousekis et al and Bourne et al sought to quantify the risk of reinjury by limb symmetry index.Fousekis 2011, Bourne 2015 Fousekis used isokinetic testing, finding that athletes with a limb symmetry index less than 85% were 4 times more likely to suffer a hamstring injury. Bourne, using a custom device incorporating the Nordic hamstring curl and a load cell, found athletes with less than an 85% LSI were 2.4 times more likely to suffer an injury while athletes less than 80% were 3.4 times more likely. This suggests that a more nuanced means of assessing strength beyond a manual muscle test is needed for determining return to sport. It also suggests that in this instance, an asymmetry should be addressed prior to returning to sport.
Another instance where data supports addressing limb asymmetries is after ACL reconstruction. Return to sport after this surgery is once again multifactorial, but limb symmetry indexes tend to be a major benchmark in the discussion typically set at 90%. A study by Grindhem et al placed athletes through a battery of tests but athletes who did not pass this battery were almost 4 times as likely to suffer a reinjury as their peers. Grindhem 2016 This study also used an isokinetic dynamometer as a means of assessing strength. Other studies advocate for an LSI of 70% prior to return to running and and PT/BW of 1.6 for males and 1.5 for females prior to returning to sport specific activities. Rambaud 2018, Myer 2008
In each instance, strength was assessed using a more quantifiable metric. It would not be common for a standard rehabilitation facility or strength coach to possess an isokinetic dynamometer however and these metrics have been established to matter more after an athlete has already been injured. In these scenarios, focused and isolated strength training is likely warranted to address the identified deficits. If there are no dynamometers, there are still means with which to estimate a limb symmetry index using equipment commonly found in globo gyms. This metric does not have peer-reviewed literature, but I would be comfortable arguing it is a better standard than a manual muscle test. If a coach has access to a standard knee extension or hamstring curl machine, a proxy for strength can still be determined. A decent testing protocol could be an athlete performing 3 sets of 6 on the machine at a prescribed RPE and using this to calculate an index. If an athlete were able to perform a set of 6 at RPE 8 at 100# on a non-injured limb and 60# on an injured limb, we now at least have a quantifiable metric from which to work. This could also be determined for upper extremity injuries such as a biceps injury using a preacher curl or a pec injury using a chest press. The key is to use a test that is sensitive enough to detect differences yet precise enough to track progress. Using a machine that selects for certain muscle groups allows for testing that is less arbitrary than a break test. The goal is to set the test so constraints are in place limiting the other means available to accomplish the task.
In each of these scenarios, there is no reason that an athlete should abstain from training. While there may be a need to focus on specific strength or hypertrophy programming for a particular muscle group, this does not mean normal programming with mild constraints cannot continue. For a lifter, they can still squat. A cap on RPE may need to be put in place so as to stay within the capacity of the healing muscle. For a sprinter, they can still participate in running drills and running, but they likely need to avoid top-end speed in the initial phases until a limb symmetry index is met.
A Case Study In Quantified Strength Deficits
There may be other instances in which strength deficits need to be addressed such as those that arise from motor weakness as the result of a herniated disc. I want to present a real world case with profound motor weakness after an injury, with a discussion of when that athlete should be allowed to train without any constraints. At the outset, I want to reiterate that normal recommendations for return to sport after the injuries listed above are at least an 85% LSI.
A 220-pound 29 year old male sustained an L3 herniated disc while sleeping on a couch that presented as radicular symptoms down his right leg. We have discussed elsewhere that herniated discs are often incidental findings, but when paired with correlating motor weakness (each level of the spine innervates a certain muscle group known as a myotome), sensory changes (known as a dermatome) or loss of deep tendon reflexes there is a much higher suspicion that the herniation is acutely contributing to symptoms. There is evidence that these herniations do heal with time, but an athlete does not need to wait for the healing to occur to continue training.Chiu 2015 Conveniently, this athlete had performed isokinetic testing 4 months prior to injury so we also have baseline data for performance.

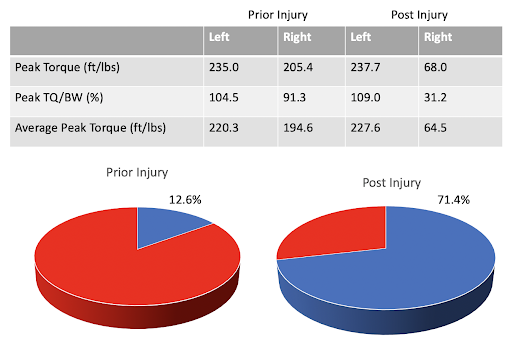
We can see an appreciable drop in strength of the right knee extensors with peak torque dropping from 205.4 to 68 ft/lbs. Still initially, this athlete presented with an 87.4% LSI. Prior to injury, there would have been no need to address this deficit and likely was as much due to the athlete’s prior training history as anything else. After, however, a 28.6% LSI was present, but the athlete was still kicking out 68 ft/lbs. For a clinician to pick this up with a manual muscle test that would mean they would have to apply more force than this in order to determine a deficit was present. As the athlete improves over time, it would be nearly impossible to detect meaningful changes beyond just “stronger.”
This raises another point in terms of strength to bodyweight ratio. If we are to use limb symmetry indexes to determine readiness for return to sport, these can give a false sense of success if the athlete is inherently weak. The athlete in this case was generating 104.5% bodyweight on the uninjured side prior to injury and had a long history of resistance training. If the same 220 pound male was only at 70% bodyweight prior to injury, kicking out 157 pounds, the 68 pound right leg would show a 57% LSI instead of 29%. While this is still a massive difference, it could give a false sense of how well the athlete is doing. It also makes the case promoted at Barbell Medicine that a general strengthening program should serve as a foundation to increase overall strength using progressive overload. When it comes to situations such as post ACL reconstruction, strength is not typically tested until at least 3 months. If an athlete has not been participating in a well designed rehabilitation program, there is also the possibility that the nonsurgical leg has become weaker during that span as well, further limiting testing sensitivity. Wellsandt 2017
Rehabilitation for this individual did involve continuing to train, but there were now constraints in place and additional means incorporated to address the identified strength deficit. Radicular symptoms resolved in a manner of weeks, but absolute load for exercises such as the squat and deadlift decreased dramatically. There was also a pronounced shift onto the left lower extremity during squatting, but the athlete was not at increased risk of injury from this, it was merely a result of a massive quadriceps deficit. As a result of the decrease in absolute tonnage for squat and deadlift, it was necessary to program in specific work for the quadriceps as well as more general physical preparation.
The main change in programming involved isolated quadriceps work 3x/week on a knee extension machine, although this could likely be accomplished with a variety of exercises that specifically address the quadriceps. Here, the weakness in the quadriceps could be directly addressed and sets were typically programmed to failure. The reason for this rationale was the overall low tolerance to load at this time and it did not take many repetitions or a high load in order to fatigue the muscle group. If the athlete had suffered a muscle injury or was post-ACL reconstruction, a rep scheme working towards 1-2 reps in reserve would have likely been prescribed. What is more, the athlete continued to train in some fashion 5 days/week through the entire process, working around the issues instead of absolute rest.
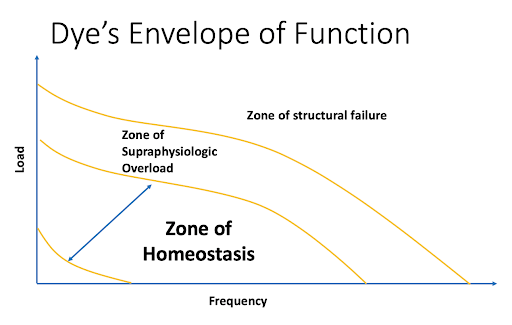
As a result of an injury, additional constraints are placed that do not allow an athlete to perform at prior levels. The goal of addressing these deficits or asymmetries is to gradually remove those constraints, and allow an athlete to return to their prior level of function. Sports such as powerlifting and sprinting are predicated upon generating maximal force, so if the capacity to generate that force has been limited by an injury, it does need to be rebuilt. This is often framed through Dye’s envelope of function.Dye 1996 Here, there is a zone of loading that is a combination of both the frequency and intensity of load needed to elicit adaptation versus remaining in homeostasis or detraining. When an injury occurs, it drops the capacity of the tissue for magnitude of load. The goal of a well-designed rehabilitation program is to return that capacity to the tissue.
Testing was performed at short increments in the beginning of rehab and the results of isokinetic testing at 4 months compared to immediately post injury are seen in Figure 5. Strength had improved in the knee extensors from 68 pounds to 140 pounds, but there is still a 54% LSI. A typical return to run cutoff for deficit is 60-80% but once again, the PT/BW ratio must be factored into the decision. The athlete is now at 64% bodyweight, up from 31%. There is also an increase in the strength of the unaffected leg by 9% from the first test post injury. If compared to the original test post injury for the unaffected leg, the LSI would now be 58%. This is stated to show how many factors are at play, and how variability in the way even isokinetic strength testing is presented can factor into how numbers are interpreted.
In practical terms, no manual muscle test is going to pick up an increase from 68 to 140 pounds of force. In three months after injury, the athlete doubled the strength in their injured leg, but in common parlance of a rehabilitation setting they would have gone from a 5/5 to a 5/5. It is also highly likely that no clinician is pushing over 100# through a manual muscle test as a means of testing knee extensors. This lack of precision has also led to the narratives of “glutes not firing” or “weak glutes” over the years as it is much easier to “break” a hip abduction test than a knee extensor.
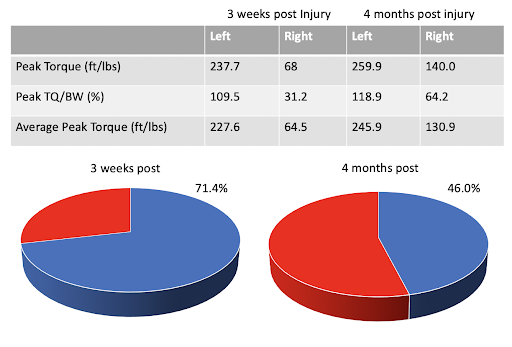
It is not until a year and a half after the initial injury that the athlete would have “passed” an isokinetic test with a 83.3% LSI. There was a year in between the 6 months and 18 month without testing so the numbers could have been achieved sooner, but now, the athlete is at 82.3% PT/BW as well. There have been obvious strength gains, over time, but there is still an asymmetry. Does this matter to a sprinter or a competitive powerlifter? Possibly. Does this matter to the average athlete who continues to train? Absolutely not.
The program for training remained the same with a focus on squats, deadlifts, and their variations followed by isolated quadriceps work via knee extensions, split squats, step ups, etc. If the athlete were instructed they need to be symmetrical prior to squatting, they likely would never return. The same could be true for the sprinter or the powerlifter. There is absolutely no reason an athlete cannot train with an asymmetry. There may need to be constraints on what that training entails due to the asymmetry in terms of intensity or an increased need to work on technique, but that should not stop training altogether.
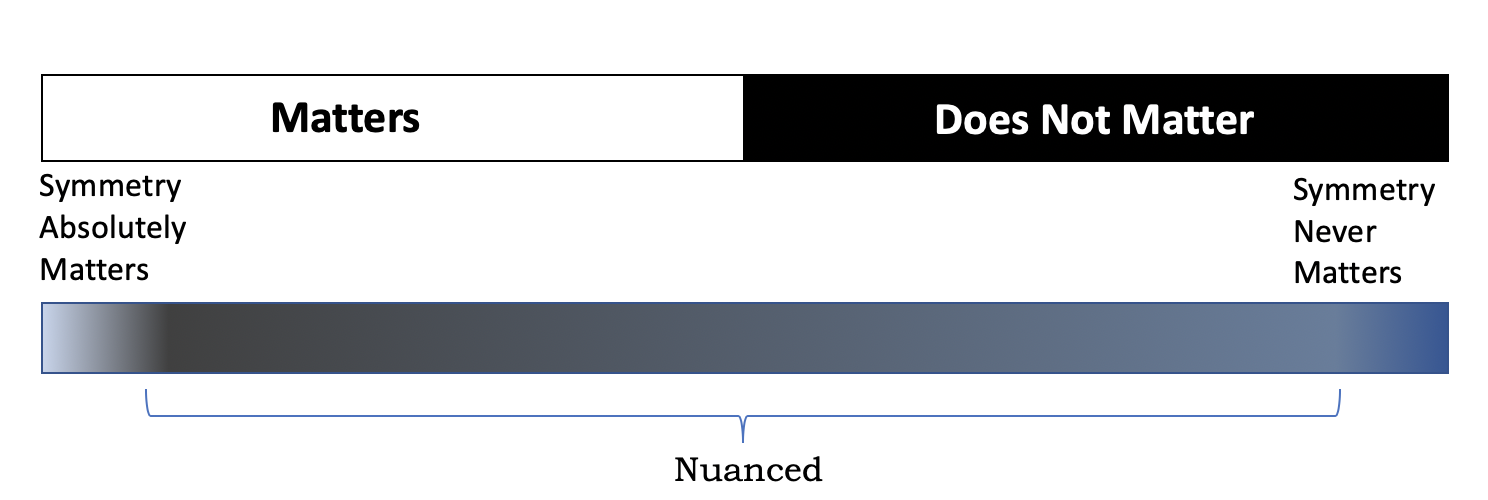
The need for the technique work is not a pass to participate in silly exercises. If anything, it often makes the case for times where a more “bodybuilding”, “isolation-style” approach is warranted. After an ACL reconstruction, there is a need for dedicated quadriceps training. After a hamstring or adductor injury, those muscles need to be specifically addressed, and machines can be quite useful in limiting the degrees of freedom and working only those muscles. There are scenarios in which asymmetries absolutely do matter. However, most arguments over the line of delineation are reduced to the top bar in figure 6 where there is only a right and a wrong answer, when in truth the bottom bar is much more reflective of the issue.
Much of the answer to whether additional work needs to transpire, or constraints need to be added to exercise prescription is contingent upon the athlete’s training history, their goals, and their current programming. If the goal is to meet the general physical activity guidelines of resistance training 2-3x/week, a large bolus of focused work to address an asymmetry is likely not needed so much as to be consistent in training. If the goal is maximum force output and there is a history of prior injury, then a more thorough strength assessment may be warranted.
The astute coach or rehabilitation professional will address a flaw seen in technique whether it be seen in squatting, jumping, change of direction. This may include cueing the athlete to perform the movement another way, changing the environment to be more ideal for learning, or it could involve performing an assessment of strength. However, that assessment needs to be sensitive enough to pick up actual strength deficits and turn them into a quantifiable issue to be addressed. The question often is not are you strong enough, but rather: are you strong enough to do what you are trying to do? When it comes to a skilled movement such as squatting, sprinting, or changing direction, working towards becoming stronger than you were prior will help to express that athleticism.
This is by no means a call to perform full body dynamometry on an athlete. It does illustrate cases in which symmetry does matter … to a point. In none of the above scenarios is the goal 100% symmetry, nor should that be the expectation. The ideal of symmetry is often portrayed in Leonardo Da Vinci’s Vitruvian Man (c. 1487), but even here, there is discussion of whether the individual portrayed represented perfect symmetry. Ashrafian 2011 There is a tendency to create a construct of “normal” that is a point rather than a spectrum. To assume everyone should squat the same way, or produce the same amount of force per kilogram of bodyweight misses two important points; 1) there is a standard deviation with every measurement of normal 2) being athletic is predicated on being able to accomplish tasks that other individuals cannot. To the first point, if the question is raised of what is “normal” range of motion, most answers would be a single number. The true answer is a range, and even then it is often predicated on the sport in which an athlete participates. “Normal” range of motion for a high level gymnast would likely be viewed as “abnormal” for a high level powerlifter.
There is nothing normal about a 3x bodyweight squat, rather it is exceptional. The second point above is more of a case for a better measurement of strength for athletes than a manual muscle test. In instances such as coming back from an injury, working towards a degree of symmetry likely matters a good deal. A program should focus on addressing this while allowing an athlete to train within the constraints of an injury.
This brings us to when an asymmetry absolutely would matter, when it is the rate-limiting step for performance, or in instances where it does increase the risk of reinjury. After a muscle injury, ACL reconstruction, or other post-surgical scenarios, asymmetries need to be both adequately tested and addressed. If a coach does not have access to a dynamometer, a quantifiable proxy should be used in place of a manual muscle test. Pushing on someone’s arm or leg is nowhere near precise enough to determine either a deficit or adequate progress after training.
A recent review found that at six months after ACL reconstruction, average side to side strength deficits was 23%.Kepley 2015 If a clinician were to wait until greater than 90% LSI to begin training an athlete, there would likely be a high degree of deconditioning happening while focused on this metric. There are still countless exercises, activities, and drills an athlete can perform while strength improves. To a bigger point, this quadriceps weakness should absolutely be a primary focus of both the rehabilitation. Isolated, focused training for strength and hypertrophy should be an integral part of the athletes programming.
For the average athlete just beginning to train, small asymmetries do not matter. The focus should be instead on increasing overall tolerance to activity and load rather than constructing problems for the athlete. We never check a child’s hip internal rotation or quadriceps strength prior to letting them kick a soccer ball, and we do not need to do this prior to letting them begin to resistance train either. The same can be said for an adolescent or adult. After injury, working towards a degree of symmetry has a place in programming, for general training purposes, it generally does not matter very much.
References
- Oliver GD, Weimar WH. Hip and Shoulder Range of Motion in Youth Baseball Pitchers. J Strength Cond Res. 2016;30(10):2823–2827. doi:10.1519/JSC.0000000000000796
- Fousekis K, Tsepis E, Poulmedis P, Athanasopoulos S, Vagenas G. Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: a prospective study of 100 professional players. Br J Sports Med. 2011;45(9):709–714. doi:10.1136/bjsm.2010.077560
- Rambaud AJM, Ardern CL, Thoreux P, Regnaux JP, Edouard P. Criteria for return to running after anterior cruciate ligament reconstruction: a scoping review. Br J Sports Med. 2018;52(22):1437–1444. doi:10.1136/bjsports-2017-098602
- Bohannon, R. W. (1987). The clinical measurement of strength. Clinical Rehabilitation, 1(1), 5–16. https://doi.org/10.1177/026921558700100103
- Kendall, F. (1993). Muscles: Testing and Function with Posture and Pain. Wulters Kluwer Health. 5th ed.
- Osternig LR. Isokinetic dynamometry: implications for muscle testing and rehabilitation. Exerc Sport Sci Rev. 1986;14:45–80.
- Greenberg EM, Greenberg ET, Albaugh J, Storey E, Ganley TJ. Rehabilitation Practice Patterns Following Anterior Cruciate Ligament Reconstruction: A Survey of Physical Therapists. J Orthop Sports Phys Ther. 2018;48(10):801–811. doi:10.2519/jospt.2018.8264
- Greenberg EM, Greenberg ET, Albaugh J, Storey E, Ganley TJ. Anterior Cruciate Ligament Reconstruction Rehabilitation Clinical Practice Patterns: A Survey of the PRiSM Society. Orthop J Sports Med. 2019;7(4):2325967119839041. Published 2019 Apr 23. doi:10.1177/2325967119839041
- Eckard TG, Padua DA, Dompier TP, Dalton SL, Thorborg K, Kerr ZY. Epidemiology of Hip Flexor and Hip Adductor Strains in National Collegiate Athletic Association Athletes, 2009/2010-2014/2015. Am J Sports Med. 2017;45(12):2713–2722. doi:10.1177/0363546517716179
- Schmitt B, Tim T, McHugh M. Hamstring injury rehabilitation and prevention of reinjury using lengthened state eccentric training: a new concept. Int J Sports Phys Ther. 2012;7(3):333–341.
- Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of Secondary Injury in Younger Athletes After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. doi:10.1177/0363546515621554
- Wren TAL, Mueske NM, Brophy CH, et al. Hop Distance Symmetry Does Not Indicate Normal Landing Biomechanics in Adolescent Athletes With Recent Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther. 2018;48(8):622–629. doi:10.2519/jospt.2018.7817
- Sanfilippo JL, Silder A, Sherry MA, Tuite MJ, Heiderscheit BC. Hamstring strength and morphology progression after return to sport from injury. Med Sci Sports Exerc. 2013;45(3):448–454. doi:10.1249/MSS.0b013e3182776eff
- Fousekis K, Tsepis E, Poulmedis P, Athanasopoulos S, Vagenas G. Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: a prospective study of 100 professional players. Br J Sports Med. 2011;45(9):709–714. doi:10.1136/bjsm.2010.077560
- Bourne MN, Opar DA, Williams MD, Shield AJ. Eccentric Knee Flexor Strength and Risk of Hamstring Injuries in Rugby Union: A Prospective Study. Am J Sports Med. 2015;43(11):2663–2670. doi:10.1177/0363546515599633
- Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. doi:10.1136/bjsports-2016-096031
- Rambaud AJM, Ardern CL, Thoreux P, Regnaux JP, Edouard P. Criteria for return to running after anterior cruciate ligament reconstruction: a scoping review. Br J Sports Med. 2018;52(22):1437–1444. doi:10.1136/bjsports-2017-098602
- Myer GD, Paterno MV, Ford KR, Hewett TE. Neuromuscular training techniques to target deficits before return to sport after anterior cruciate ligament reconstruction. J Strength Cond Res. 2008;22(3):987–1014. doi:10.1519/JSC.0b013e31816a86cd
- Chiu CC, Chuang TY, Chang KH, Wu CH, Lin PW, Hsu WY. The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clin Rehabil. 2015;29(2):184–195. doi:10.1177/0269215514540919
- Wellsandt E, Failla MJ, Snyder-Mackler L. Limb Symmetry Indexes Can Overestimate Knee Function After Anterior Cruciate Ligament Injury. J Orthop Sports Phys Ther. 2017;47(5):334–338. doi:10.2519/jospt.2017.7285
- Dye SF. The knee as a biologic transmission with an envelope of function: a theory. Clin Orthop Relat Res. 1996;(325):10–18. doi:10.1097/00003086-199604000-00003
- Ashrafian, H. Leonardo da Vinci’s Vitruvian Man: a renaissance for inguinal hernias. Hernia 15, 593–594 (2011). https://doi.org/10.1007/s10029-011-0845-6
- Lepley LK. Deficits in Quadriceps Strength and Patient-Oriented Outcomes at Return to Activity After ACL Reconstruction: A Review of the Current Literature. Sports Health. 2015;7(3):231–238. doi:10.1177/1941738115578112
