Diabetes is among the most common conditions encountered by patients and doctors today, affecting nearly 1 in 11 people worldwide. Unfortunately, it remains poorly understood by the general public, and even among many healthcare professionals. There are many different kinds and causes of diabetes, but today we will focus on common type 2 diabetes mellitus. We will explain the disease and treatments that make the biggest impact in a simple and understandable way. [Roden 2019]
Human metabolism describes how we convert the calories we eat and drink into chemical energy that our body can use. This chemical energy drives our heartbeat, breathing, kidneys, liver, and many other bodily processes that happen all the time. Our muscles can also use this energy for general physical activity or exercise. We therefore always require a steady supply of fuel in the bloodstream. This can come directly from the diet, or from stored energy reserves from the liver or from body fat. Carbohydrates from the diet end up in the blood as glucose, fats end up in the blood mostly as triglycerides, and proteins end up in the blood as amino acids. The body has multiple finely-tuned ways to maintain healthy blood levels of these substances by balancing their storage and release throughout the day and night, whether we are eating or not.
The Basics of Blood Sugar Regulation
After we eat a meal, cells in the pancreas have sensors that detect an increase in blood glucose or amino acids. These are called “beta cells”, which respond by releasing a hormone called insulin. Insulin shuttles glucose, amino acids, and fats from the bloodstream into cells for use or storage. Insulin also shuts down the release of glucose and fats from storage reserves in the liver and body fat, since there is no need to use up fuel reserves when energy from food is coming in. By simultaneously shuttling glucose into cells and blocking glucose release from the liver, insulin can potently lower blood glucose back down to normal.
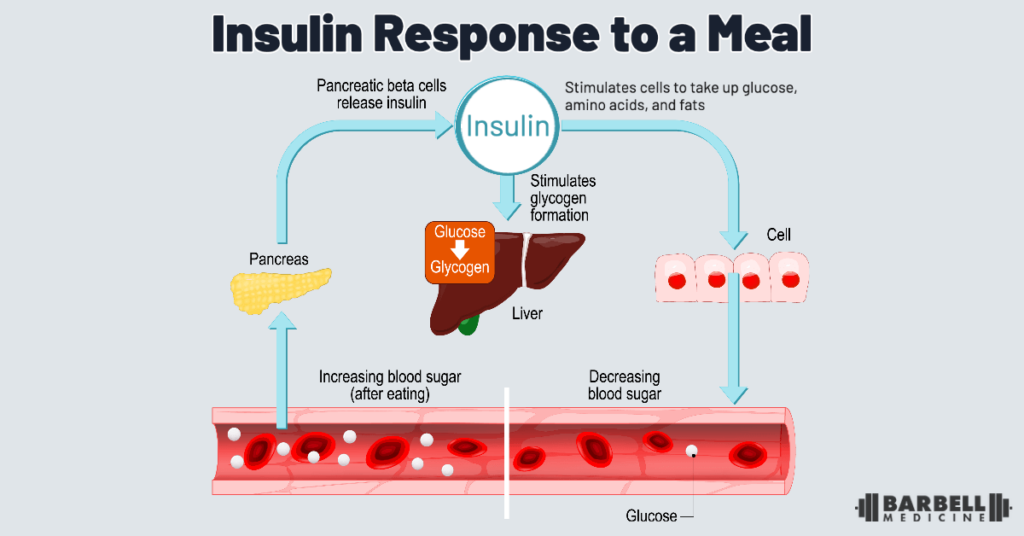
The immediate increase in insulin within minutes after a meal is known as the “first-phase response. If blood glucose remains high, the “second-phase response” involves ongoing insulin release continues lowering blood glucose in the subsequent hours after a meal.
Extremely high blood glucose levels directly injure beta cells, a phenomenon called “glucotoxicity”. This impairs their ability to sense blood sugar increases and the first-phase insulin response. This beta cell dysfunction is one contributor to diabetes mellitus, where blood glucose regulation is impaired. Other contributors involve resistance to the effects of insulin in the rest of the body, or losing the ability to produce insulin altogether. These concepts will be important when discussing testing and treatment for diabetes in later sections.
The Basics of Fat Storage
When we consume more calories needed to fuel our bodily processes, we store this excess energy in fat cells, also facilitated by the action of insulin. This provides a critical backup energy source for survival, although too much body fat can cause problems too. Body fat is preferentially stored under the skin, known as “subcutaneous fat”.
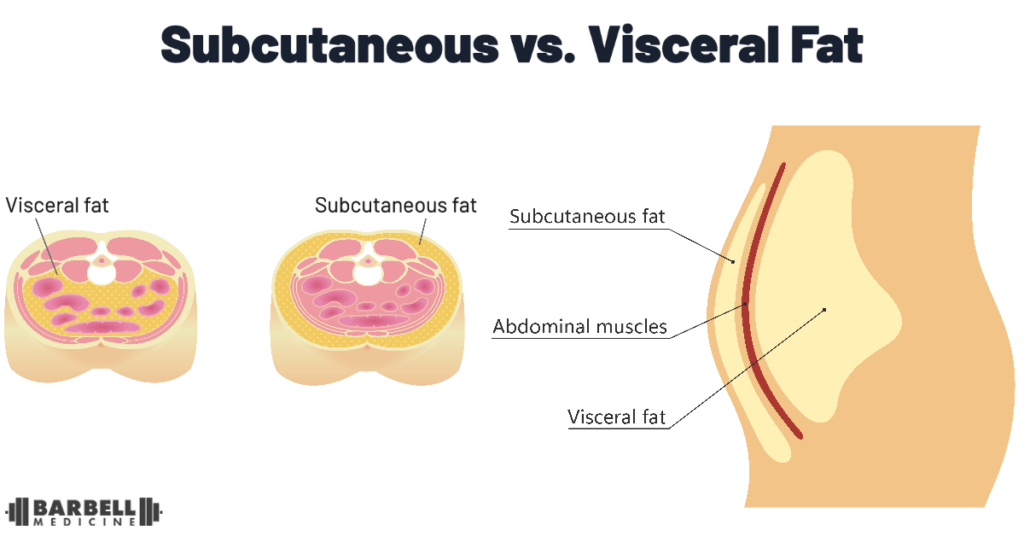
Fat cells have a limited capacity for storage. Health problems begin to develop when this limit is exceeded. Each person’s fat cells have a different limit based on their genetics, diet, physical activity habits, certain medications, and many other factors. Once a person’s fat cells under the skin reach their size limit, they signal the creation of new fat cells. Different people also have different abilities to produce new fat cells, similarly related to genetic differences. [Haczenyi 2018] These concepts have been collectively called the “Personal Fat Threshold”. [Taylor 2015]
When at maximum capacity, fat cells become stressed, inflamed, and stop listening to the signal of insulin. They stop taking in any excess calories floating in the blood in the form of glucose and fatty acids. This condition is called “insulin resistance”. [Kim 2015] When there is no more room in fat cells under the skin, the excess calories remaining in the bloodstream end overflowing into other locations. It gets deposited as “belly fat” in and around organs like the liver and pancreas, and can also end up abnormally deposited in muscle. [Frayn 2002, Taylor 2013].
The Problem of Belly & Muscle Fat
When the liver develops insulin resistance due to excess belly fat (known as “fatty liver disease”), it stops listening to the signal of insulin that would normally suppress it from releasing glucose from storage. This contributes to the high blood sugar levels seen in when “fasted” first thing in the morning.
When fat is deposited abnormally within our muscles, they similarly become resistant to the effects of insulin. As a result, they stop taking up glucose from the blood and using it as fuel, particularly when a person is not sufficiently physically active. This further exacerbates high blood glucose, especially after meals.
Fat storage in the pancreas interferes with normal function, adding to the glucotoxicity described above. Impairments in the normal first-phase response of insulin release after a meal further exacerbate high blood glucose levels. As a result, the pancreas must increase insulin levels all the time — even when the person has not eaten — in an attempt to normalize blood glucose levels. It may be able to compensate temporarily, but without intervention the beta cells become more dysfunctional and die over time.
Some people reach their personal fat threshold with relatively little body fat, leading to the development of health problems sooner, whereas other people can store a lot of fat without developing many immediate health problems. In extreme conditions, an inability to store fat under the skin known as “lipodystrophy” means reaching maximum fat storage capacity despite not having very much body fat at all. This leads to severe insulin resistance and the same health problems typically associated with higher body fat levels, such as diabetes, high blood pressure, and abnormal blood cholesterol, despite having extremely lean arms and legs.
Overall, type 2 diabetes mellitus results from a combination of 1) beta cell dysfunction, leading to impairment in first-phase insulin response and eventual death of these cells, and 2) insulin resistance in the tissues due to exceeding one’s personal fat threshold, leading to fat deposition in the liver, pancreas, and muscle. With all of these issues occurring, blood glucose can rise high enough that it becomes apparent on blood tests or through symptoms like excessive urination, dry mouth, blurred vision, fatigue, or unintentional weight loss. [Bergman 2023]
Armed with this knowledge and a waist circumference measurement, we will move on to testing and treatment strategies for type 2 diabetes in upcoming parts.
Take-Home Summary
- The beta cells of the pancreas sense increases in blood glucose (and/or amino acids). They respond with an immediate “first-phase” release of insulin, and then through a more prolonged “second-phase”. Insulin shuttles nutrients into cells for use or storage, and suppresses the release of glucose and fat from storage sites. This results in a lowering of blood glucose levels back to normal. Extremely high blood glucose levels directly damage the beta cells and their first-phase response; this is known as “glucotoxicity” and contributes to the development of diabetes.
- Excess energy from calories in the diet is stored as body fat, preferentially under the skin. Fat cells have a limited capacity for storage. When these are full, we have a limited ability to generate new fat cells. These limits are variable between people based on individual genetics, diet, physical activity, certain medications, and other factors. This is why people develop diabetes and other associated health problems with different levels and distributions of body fat.
- When a person reaches their individual limit for fat storage under the skin, fat cells become inflamed, dysfunctional, and resistant to the signals of insulin. This leads to the accumulation of energy in the bloodstream (high glucose and fats in the blood), which “overflows” into belly fat in the liver and pancreas, as well as in muscle.
- Fat stored in the liver, pancreas, and muscle cause these tissues to become insulin resistant and dysfunctional. This also contributes to the high fasting blood sugars and excessively high blood sugar increases after meals that characterize type 2 diabetes. They also contribute to other findings of insulin resistance, such as high blood pressure and abnormal blood cholesterol, among others.
Thank you to Tom Campitelli for his assistance in editing this article.
