Pain in the front, side, or back of the hip are common complaints within the lifting community. A combination of factors are typically involved when experiencing pain or limitations in training, rather than “just one thing” that needs to be addressed. The hip is a complex region that does not have a clear way to classify pain issues. As with other joints, a combination of symptoms, orthopedic tests, and imaging tests like X-rays are often used to isolate a cause of pain or limitations. The issue with this approach is that while we can use it to confidently rule out certain problems, it has a very limited ability to isolate and confirm a single source of symptoms.
For example, in an individual with pain in the front of their hip, many of the special examination techniques will be positive regardless of any underlying issues, X-rays or other imaging tests commonly reveal abnormalities in all athletes, not just in those with pain. This murkiness leads to diagnoses such as “femoroacetabular impingement”, “hockey hip”, “Gilmore’s groin”, “athletic pubalgia”, and a host of others that are almost impossible to differentiate by individual clinicians. This further leads to confusion on the part of the athlete, as complicated medical labels are assigned without clear direction on how to address what they are experiencing.
This article series aims to provide a guide to address common issues that may arise when training with hip pain. It is by no means exhaustive, and if an individual is unable to achieve relief with the recommendations, they can reach out to the Pain and Rehabilitation team for consultation and further assistance. This first section will be a bit more “science heavy”, which will likely be more useful for coaches and clinicians, whereas the following articles in the series will provide much more practical advice for lifters experiencing hip pain.
The Biology Side of Things
The hip is a ball and socket joint that allows for a high degree of movement. There are 21 muscles crossing the joint that facilitate this movement. All of these muscles work together to set up and perform exercises like the squat, bench press, and deadlift that form the foundation of training for most of our readers. The joint consists of two bones, the femur and a hemipelvis. The femur is the “thigh bone”, and the head of the femur is the “ball” part of the joint. The hemipelvis is a fusion of three bones: the ilium, ischium, and pubis, which come together to form the “socket” known as the acetabulum. The “ball” (head of femur) thus fits into the “socket” (acetabulum) to form the joint. Around the outer edge of the acetabulum is a layer of fibrocartilage that serves to seal the joint known as a labrum.

There is extensive variation in the demands and adaptations of the hip in sports, occupations, and general activities of life. It is expected that different individuals will demonstrate differences in hip function, strength, range of motion, and imaging findings based on the demands — and thus adaptations — of their chosen activities. For example, we would expect to find very different adaptations and function between the hips of hockey players and swimmers. With respect to the barbell athlete, we don’t have studies on what constitutes “normal” range of motion, strength, etc. Many individuals start resistance training later in life, and much of the adaptive changes to our anatomy occur through the adolescent years, with subtle changes continuing to occur throughout the lifespan as different types and magnitudes of stress are applied.
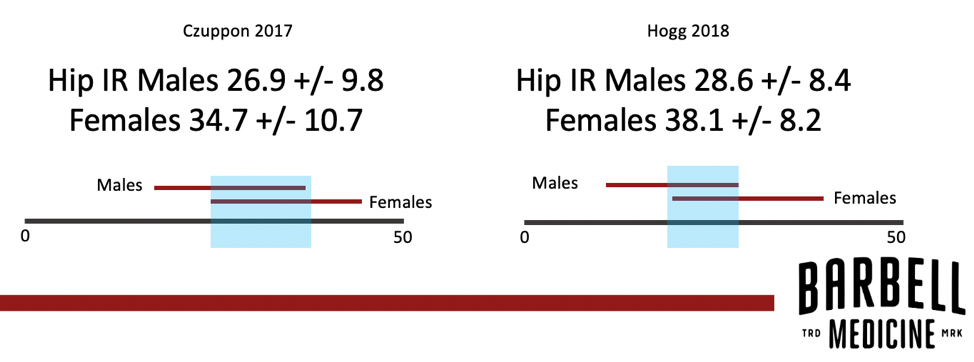
Examining range of motion for the hip joint illustrates the variance between individuals. In one study, 120 pain-free individuals were assessed to see if they had more internal or external rotation at the hip. More external rotation was observed in 47.5%, more internal rotation was observed in 13%, and 39.5% showed equivalent external and internal rotation range of motion. Kouyoumdjian 2012 Based on these data it would be difficult to argue for a strict “normal value” for hip rotation range of motion across all individuals. Other studies corroborate the variability in these measurements and illustrate the variance in what constitutes normal range of motion. A study of freshmen collegiate athletes reported normal hip internal rotation was 26.9 degrees in males and 34.7 degrees for females. Czuppon 2017 However, this defines “normal” as a single discrete value. In the study, the standard deviation of normal range of motion for both genders was approximately 10 degrees, indicating a much broader range than just defining anything above or below that single point as either “excessive” or “limited” range of motion. Another study of collegiate athletes had similar overall findings, but they also found variance between different sports. Hogg 2017 It therefore appears that there is no generalizable “normal” for all humans. There is even evidence that individual range of motion is a snapshot with time-dependence, as baseball players demonstrate changes in their hip range of motion over the course of a season, likely based on a number of factors including their competitive demands. Zeppeiri 2015
Normal hip strength is also often a misnomer with “weak” glutes, hamstrings, or quadriceps being blamed for a myriad of problems. There is even the myth of “gluteal amnesia”, as though people can somehow forget to fire their gluteal muscles, or that this firing under normal circumstances should be a cognitive task. The primary issue with these arguments can be found in assessment methods. There are two main ways gluteal strength is typically assessed in practice; a manual muscle test or through functional analysis. Manual muscle testing involves an examiner resisting various muscle actions and grading the individual’s strength on a scale of 1 to 5 out of 5. This technique is not an effective means for grading strength, as the difference between a “4/5″ (able to resist against gravity with moderate pressure) and “5/5” (able to resist against gravity with strong pressure) are both predicated on what is “moderate” or “strong.” I’ll let you in on a little clinical secret: many clinicians will vary their pressure in order to “break” the position, and therefore be able to say an individual is weak in the tested muscle group.
If gluteal strength is assessed with a functional task such as observing someone squat, jump, or run, there is an assumption that “weakness” in one area correlates with performance in another. This fails to account for the skill required to perform certain movements. If an individual has not practiced squatting, it is unsurprising that they may be unable to perform a technically beautiful squat. The same can be said for activities like a lunge or a jump that are included in common screening tests. If “gluteal amnesia” were as prevalent as many clinicians claim, there would surely be more evidence of it in the peer-reviewed scientific literature:
There is also a tendency to view movement that deviates from an idealized normal as indicative of an underlying problem. A discussion of screening tests is beyond the scope of this piece, but suffice to say that there is no good evidence that moving differently from an arbitrary pattern is indicative of gluteal weakness. The common example referenced here is a Trendelenburg test which typically involves an athlete standing on one leg, flexing the hip on the opposite side to 30 degrees, and elevating the pelvis on the non-stance leg “as high as possible,” holding it for 30 seconds. Failure to do so is often deemed a “Trendelenburg sign” and supposedly indicates weakness in the hip abductors, despite the fact that we have studies that call the validity of this test into question. McCarney 2020, Kendall 2013 The term “weak” is also nebulous, as “sufficient” strength will differ between an athlete attempting to run a half marathon and an athlete attempting to deadlift three times their bodyweight. While gluteal muscles can become weak like any other muscle, this should be viewed relative to what the person is attempting to perform, rather than relative to an idealized “normal”.
There is also some evidence that counters these ideas as well, with some studies finding an increase in gluteal activation in individuals experiencing pain. Dwyer 2013 Marshall 2011 Once again: normal is a spectrum, and is more likely predicated on what your current level of fitness is, what internal and external stresses you are experiencing, and your goals for movement and performance. While an individual squatting three times their bodyweight would certainly be considered “strong” by most standards, in most instances they would likely not fare well converting that hip strength into a half-marathon performance. Ideas about glutes being weak, “asleep”, or forgetful are not based in scientific plausibility. It is often not about whether you are strong or weak but rather are you strong enough to do what you are trying to do. In these situations we are better served by emphasizing capacity over raw values, especially when those values are often arbitrary.
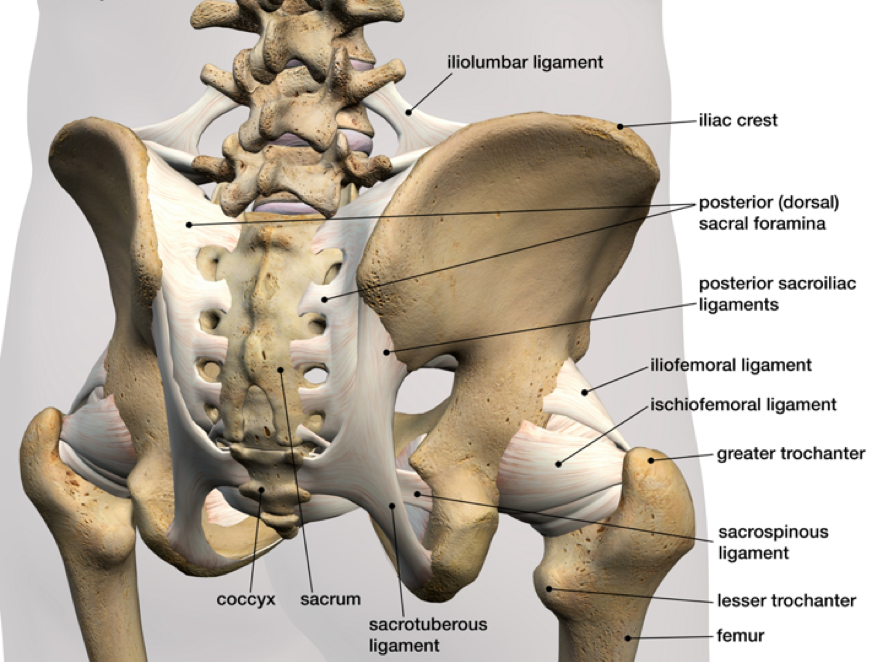
Lastly, we will address the common idea of hips being “out” (with reference to a prior post at the Logic of Rehab). While this narrative is not specifically about the hip joint itself, it often arises from an individual’s perception of symptoms being in their hips. The joint actually being referred to in these instances is the sacroiliac (SI) joint. Even here, the narrative of a rotated or “out of place” hip joint (ilium on sacrum) causing dysfunction is completely unfounded. There are three points that will hopefully explain why this narrative is wrong, and potentially harmful to athletes.
- The ilium and sacrum do not move on a perceptible level
- The special tests we have to determine movement are inaccurate and unreliable
- Words have a lasting meaning on an athlete’s perception of their situation
Continuing education classes and prominent textbooks teach that rotation or movement of the bones that make up the hemipelvis (known collectively as the “innominates”) are a viable cause of athlete symptoms. This is patently wrong. Decades of accumulated studies have found a lack of movement in this joint. Nagamoto et al found less than one degree of movement in the SI joint, far below any perceptible level from a clinician’s examination. Nagamoto 2015 A systematic review by Goode et al found 8 degrees of movement in the Z-axis, 2.2 degrees in the X-axis, and 4 degrees in the Y-axis. Goode 2008 The authors of the paper went so far as to conclude:
“Motion in the SIJ is limited to minute amounts of rotation and translation suggesting that clinical methods utilizing palpation of diagnosing SIJ pathology have limited utility.”
There are two points in that sentence that are worth expanding upon: the use of palpation (touching and feeling an area during examination) and the diagnosing of SI joint pathology. When palpation is studied for the SI joint, there are two major themes that emerge: 1) there is a high level of normal variance within the joint and 2) clinician palpation has poor accuracy and reliability. A cadaveric study found a side to side difference of up to 11 degrees asymmetry of pelvic landmarks, and up to 16 millimeter differences in innominate height. Preece 2008 Identifying up to 11 degrees of asymmetry when the joint itself has only been shown to move 8 degrees seems to call into question our ability to use anatomical landmarks to accurately identify real problems during a physical exam. Even with natural asymmetry, clinicians have difficulty identifying the basic anatomical landmarks. Another group looked at the reliability of palpation and found only a 48% agreement among trained clinicians. Robinson 2008
One of the main landmarks used in ideas about hip joints being “rotated” is the posterior superior iliac spine (PSIS). It is plausible that such a large landmark could be useful, until we find that clinicians can be on the landmark while palpating many different areas. One study found very poor reliability for palpating the PSIS (kappa = 0.27), far below what would be necessary for clinical utility. Cooperstein 2016 Another took this a step further by examining the reliability of bony landmark asymmetry and found multiple landmarks possess no good reliability. Stovall 2010
If the SI joint itself is inherently stable (read: it does not move), and clinicians cannot accurately palpate even the largest landmarks, then there is no convincing evidence to substantiate that a “rotated hip” is a major cause of symptoms. Even if this were the case, there is nothing a clinician can do to manually “reset” the joint. A 1998 study using advanced X-ray technique known as Roentgen stereophotogrammetric analysis found less than a millimeter of translation along any axis, and less than a degree of movement at the joint. Tullberg 1998 There is no doubt that some clinicians will claim that the authors did not use their specific technique; we would invite those clinicians to publish their findings in a reputable journal. Until then, there is no good evidence for resetting the SI joint with any manual therapy technique.
As for orthopedic special tests, most clinicians readily turn to Laslett’s 2008 paper on clusters, which contains an interesting insight [emphasis added]: Laslett 2008
“The manual therapy literature is awash with books, chapters, and papers on the treatment of the sacroiliac joint. Most of these treatment methods are based explicitly or implicitly on the presumption that some biomechanical malfunction or dysfunction causes either the SIJ or other tissues to provoke the pain of which the patient complains. This hypothesis is fragile indeed, since the means by which such dysfunctions are identified rest upon a flimsy evidential base, disputed by published data showing tests for SIJ dysfunction to be unreliable and invalid.”
Other studies of single-leg stance and straight leg raise maneuvers for detecting motion in the joint that also show less than one degree of motion. Kibsgard 2014, Kibsgard 2017 Using a skill with low utility to identify movement that may be unrelated to pain is dubious.
Finally, there is not a gold standard to determine whether pain is actually originating from the SI joint. A distinction needs to be made between pelvic dysfunction and pelvic pain. Among athletes presenting with posterior pelvic pain, it is unclear how much or how often the SI joint is the pain generator. Among individuals with no pelvic or hip pain, studies have found evidence of SI joint degeneration of up to 65.1%, with 30.5% of them showing “substantial degeneration.” Eno 2015 Once again, these individuals did not have any symptoms.
If such pelvic “abnormalities” are readily prevalent in the asymptomatic population, it is hard to confidently deem it to be the root cause of a patient’s pain. We have established that 1) special examination tests lack validity, 2) palpation sucks, and 3) the involved joints do not move. As a result, we suspect that what clinicians are trained to see influences what they believe to be the problem. This is akin to the phenomenon of pareidolia, in which people see or hear what they expect to see or hear — even when no true signal exists. The classic examples include seeing a man on the moon or Jesus on a piece of toast. If an individual is primed to see or hear a stimulus, e.g. trained in school via diagrams of SI joint movements, many will “find” those movements whether they are present or not. A 2001 study demonstrated this: undergraduate students listened to a recording to detect Bing Crosby’s “White Christmas.” Merckelback 2001 Approximately 30% of the students reported being able to hear the song when there was nothing but noise present.
Narratives that athletes have their hips “out of alignment”, “rotated”, “nutated”, or in line with Mercury while it is in retrograde, all have the same level of evidence: none. Yet, because of the normal information asymmetry between clinicians and athletes, many people experiencing symptoms do not know that. They are given a problem (that does not exist), to which there is no solution (prior parenthetical explains why). Part of the role of returning an individual to prior levels of function is guiding the path, and wading through many of the narratives athletes have previously received.
In the following articles, we will shift to a more practical discussion of four primary categories of hip pain most common in athletes and provide advice for management. These general guidelines should allow an athlete to make the decision to train “through”, or “around” an injury and provide tools to track progress. These categories include tendinopathies, impingement, muscle injuries, and osteoarthritis. Each of these have unique features and treatment focus, which will be expanded upon in coming sections.