In the first two installments of this article series we discussed the science of hip pain and management strategies. In this article, we’ll discuss the topic of muscle injuries – these are colloquially known as a “muscle strains”, but that term is a better description of the mechanism of the injury than a description of the injury itself. Mueller-Wohlfahrt 2013
An athlete who experiences a sudden “pop” or immediate pain after a repetition likely falls into the “muscle injury” category. There are two situations that would warrant immediate evaluation after this has occurred:
- In an instance where an athlete feels a “pop” and there is a noticeable deformity in the muscle afterwards, they should seek consultation with a qualified sports medicine physician. The criteria and candidacy for surgical repair involve many factors, but if the athlete is a good candidate, the sooner they can be evaluated and scheduled, the sooner the rehabilitation process can begin.
- The second scenario is with adolescent athletes who experience a “pop.” In the developing skeleton, adolescents are more predisposed to avulsion fractures, where a portion of the bone pulls away instead of the muscle being torn. In most instances, these are managed conservatively, but it does change the time course and aggressiveness of rehabilitation.
The cause of muscle injury, like most other injuries, is complex. The mechanism is the strain where there are greater eccentric muscle forces than the tissue can bear. This causes a sudden tear in the muscle fibers to varying degrees. This does not only happen under maximum effort, as there also appears to be a programming effect on injury risk as well. In a study of hamstring injuries in the NFL over 10 years, the vast majority of injuries occurred during the first 4 weeks of the preseason. Elliot 2011 There are multiple factors that may contribute here, as it may be related to players working harder to attempt to make the roster, but it also is a time where players are going through a shift from their off-season training to the suddenly higher demands of pre-season workouts. The same phenomenon has been seen in Australian Rules Footballers where the amount of high-speed running was related to the likelihood of suffering a hamstring injury. Duhig 2016 While there are no specific studies looking at the rate of muscle injuries in resistance training, there does seem to be two driving principles that can increase risk:
- Being exposed to a large, sudden increase in training volume
- Having a large volume of maximum intensity training in a short period of time
All of this is relative to the individual athlete, as what would constitute a “large” change is contingent upon the athlete’s overall foundation and training history. There also seems to be a relationship between anabolic steroid use and muscle injuries. In two different case studies, use of anabolic steroids was associated with muscle injury with 96% of individuals in one cohort reporting steroid use prior to injury. Schutzel 2014, de Castro Pochini 2013
One of the first questions that always arises after an injury involves the need for imaging tests. Outside of the cases mentioned above involving obvious deformities or adolescent injuries, there is not much utility for imaging when determining the course of care after a muscle injury. In two studies, the addition of imaging did not add utility in the determination of when an individual could return to sport. Jacobsen 2016 Wangensteen 2015 This was further confirmed in a systematic review that concluded “there is currently no strong evidence for any MRI finding in predicting hamstring re-injury risk.” von Heumann 2017
Evidence suggests that many factors do not yield much predictive value in terms of return to sport. The current best evidence for hamstring injuries suggests that the following factors are associated with an increased likelihood that an athlete will be out of competition for over 4 weeks: Guilodo 2014
- subjective pain greater than 6 on a scale of 1-10
- pain with routine activities of daily living for greater than 3 days
However, athletes do not need to abstain from training during that time and should be working on the fundamentals of rehabilitation, with the goal of transitioning through participation in training, to practice where loads return to normal levels, and finally to competition. Even if symptoms limit participation in some activities, there is often still plenty to address in terms of athleticism to facilitate return to sport.
A graded return to heavy training and competition is imperative for multiple reasons. In a study of athletes who had returned to sport after hamstring injury, there were still 20% differences in the size (by cross-sectional area) of injured and uninjured legs. In addition, there were 10% strength deficits between sides, and even 6 months post-injury there were still 4-5% differences side-to-side. Sanfillippo 2014 Post-muscle injury is a situation where, to a degree, symmetry does matter. In one study, individuals returning to sport with a limb symmetry index (LSI) of less than 85% were four times more likely to suffer a re-injury. Fousekis 2011 In a separate study, athletes with less than 85% were 2.4 times more likely, while those less than 80% were 3.4 times more likely to experience re-injury. Bourne 2015
How Do We Address This?
The best evidence for the conservative treatment of muscle injuries is with eccentric-oriented exercises such as the Nordic hamstring curl, Reverse Nordic curl, and Copenhagen adductor exercise. A systematic review demonstrated an overall reduction in risk for hamstring injuries in athletes participating in eccentric-based training, as long as they adhered to the program. Goode 2015 It should come as no surprise that in order for exercise to work, it actually needs to be done. These findings are extrapolated from studies looking at athletes participating in high-speed running, not resistance training, but they still offer an operational plan for getting started.
Resistance-trained athletes experience different types of force than athletes in high-speed running, but the overall methods for rehabilitation are the same. The only difference being resistance-trained athletes may benefit from isolation, bodybuilding-style work as part of rehabilitation in order to regain any lost strength. It can also be framed through the lens of either percentage or RPE-based training, as part of the issue is the magnitude of force. Once symptoms are under control, an athlete can begin participating in training more, but it should be with the understanding that there are still constraints on what they should perform. For example, if the athlete has 100% strength on one limb and 80% on the other, they are likely fine to train with less than 75-80%, but pushing beyond that would likely exceed the capacity of the injured limb.
Much time is spent at Barbell Medicine discussing the correlation between tissue damage and symptoms. In the instance of muscle injuries, pain symptoms typically resolve before an athlete is truly ready to return to high-level training. This can create a false sense of security where an athlete may be doing more than they are actually ready to do. An athlete will often return to prior training because they feel good, only to have a setback because they increased their workload beyond their capability at that time. A cycle of frustration then emerges as an athlete starts to improve, feels good, then has another setback. The goal of a well-designed rehabilitation program is to reduce the risk of those setbacks and help an athlete return to and exceed prior levels of performance.
At the beginning of the rehabilitation process, a conversation regarding training modifications needs to transpire. If an athlete cannot spend as much time in top-end training, there is utility in the addition of different exercises to maintain fitness. If a heavy competition-style deadlift needs to be removed from the program during a month of rehab, isolated hamstring work, back extensions, and single-leg work can take its place for this temporary period. If a groin injury prevents heavy, full-range squatting, then knee extensions, leg presses, and split squats can find a place in the program. There are instances where an athlete can train “through” an injury, and instances where it is more beneficial to train “around” an injury. In the case of muscle injuries, training “around” while the tissue heals and strength is regained reduces the risk of setbacks. Now, let’s discuss some specific cases.
Hamstring Muscle Injury
For a hamstring muscle injury, the exercise of choice is the Nordic Hamstring Curl (fig 1).
An athlete can secure their ankles under a rack or bar, while attempting to keep their trunk upright, slowly fall forward. This is a very challenging exercise and the athlete will feel significant tension in both hamstrings. The normal prescription here is 4 sets of 6 repetitions and athletes can work on this every other day, allowing for recovery in between.
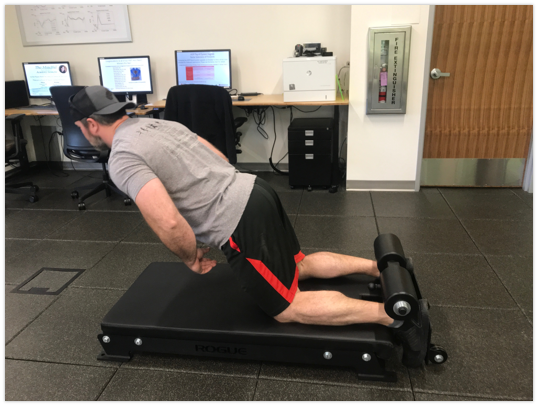
Athletes can also use machine hamstring curls in the gym. This has the additional benefit of allowing an athlete to work single-leg strength and compare the injured leg to the uninjured leg. An athlete can use the principle of reps in reserve (RIR) or rate of perceived exertion (RPE) to estimate a limb symmetry index. If an athlete can perform 8 reps at RPE 8 using 100 pounds on their unaffected leg, but only 80 pounds on their affected leg, we can estimate a limb symmetry index of 80%. Once again, the goal is not necessarily to achieve 100% symmetry prior to return to activity, but a goal of greater than 90% should likely be achieved prior to competition. [Note: there are instances where this would not be the case contingent upon an athlete accepting risk.]
These recommendations are primarily for barbell-based athletes. Those who suffer a hamstring muscle injury as a result of sprinting may require other exercises as well. They also certainly need a gradual reintroduction of high-speed running prior to returning to competition. The program can begin with form running drills and jogging then progress to picking up intensity from a rolling start. Finally, progressing to working on maximal speed from blocks and full-speed accelerations.
Groin (Adductor) Muscle Injury
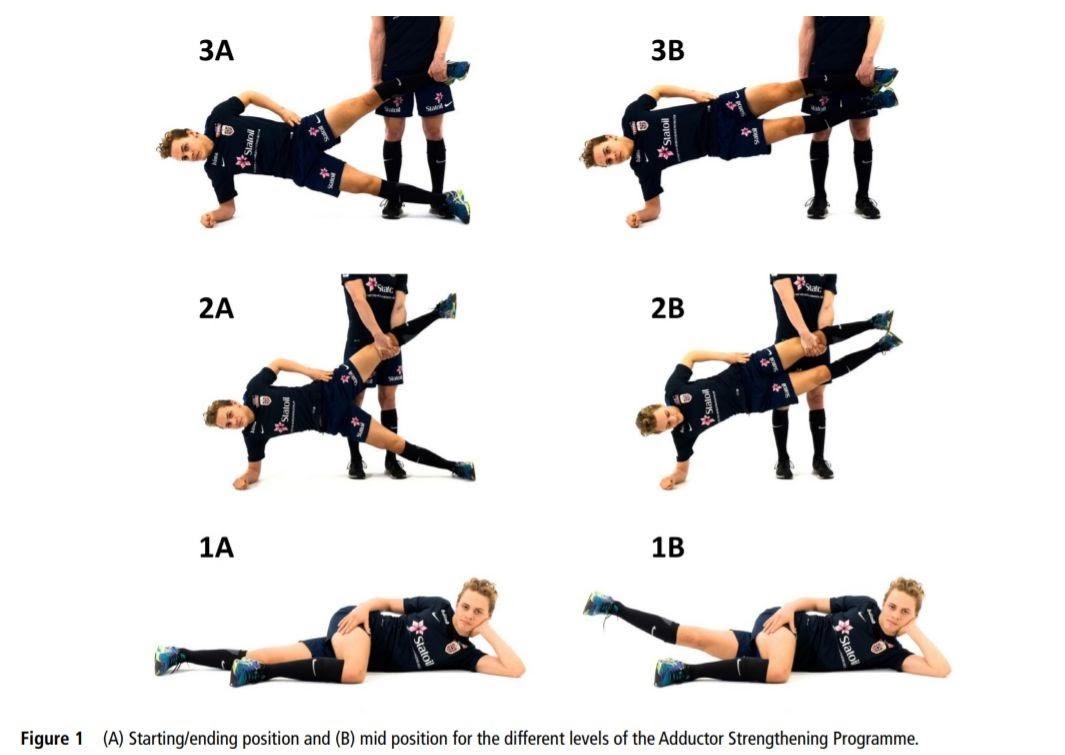
For a groin muscle injury, the exercise of choice is the Copenhagen Adductor Exercise (Fig. 2). Haroy 2019 This exercise has different degrees of difficulty (compare exercise versions 1, 2, and 3 in the figure) with the goal of finding one sufficiently hard for the athlete. The objective is still to work slowly through a large range of motion, and typically 4 sets of 8 repetitions is sufficient here. In addition, an athlete can use a seated adduction machine, lateral lunge, or Cossack squat to provide further stimulus to the adductor. Implementation of the Copenhagen protocol resulted in a 41% reduction in the incidence of groin injuries in soccer players.
Hip Flexor and Quadriceps Muscle Injury
Hip flexor injuries are a broader group as it is more difficult to directly isolate the movement using resistance. The exercise of choice here is the Reverse Nordic Curl (Fig 3), where an athlete is in the tall kneeling position and instead of falling forward, falls back. Alonso-Fernandez 2019 A stretch will be felt across the front of the hip joint. A typical scheme here is 4 sets of 6 repetitions, again performed every other day. Supplemental work here can include exercises such as a rear-foot elevated split squat, trunk work, or hanging knee or leg raises. The goal in each instance still being to work through full range of motion in a slow, controlled manner.

Lastly, there are quadriceps injuries lacking direct research to recommend a specific exercise. Under our heuristic of using eccentric exercises with a large range of motion, an athlete could perform an eccentric-focused leg press, where they push out with two legs, then remove one leg to come down slowly on the affected leg. The same movement could be performed on a knee extension machine. If an athlete trains in a powerlifting-style gym without extra equipment, a single-leg squat or split squat with a focus on the eccentric could be useful. For each injury, part of the process is determining equipment access and designing the program to suit those specific needs of the athlete.
Return to Training and Competition
Return to training and competition from muscle injuries should be an informed decision based upon the objective metrics of limb symmetry, as well as subjective feel of the athlete. The current consensus is that an athlete should be psychologically ready to return as well as exposed to sport-specific positions without increases in symptoms. van der Horst 2017 This is basic advice, but in terms of a strength athlete returning to competition training it bears mentioning that there should be a gradual ramp back into training. When returning to full training, we re-frame the use of RPE from “could” you do two more reps, to “should” you do two more reps. The subtle difference here leaves a slightly larger reserve as an athlete gets back to heavier loads.
There are other general factors at play here, such as the timing of the next competition and the level of that competition. A conversation regarding risk versus reward should take place; for example, if an athlete’s financial income is contingent upon placing at an upcoming competition, more risk may be accepted. If another athlete has signed up for a local meet and is still experiencing symptoms at lower weights when two weeks out from competition, the social media likes for going 4/9 are not likely worth the extended frustration of attempting to return too soon.
In today’s article we’ve discussed the approach to managing acute muscle injuries including the hamstrings, groin (adductors), hip flexors, and quadriceps, as well as how we progress towards return to sport using limb symmetry criteria. In our next article we’ll move on to discuss a complex topic: Femoroacetabular Impingement Syndrome (FAIS).